For as long as I can remember, I have considered myself a headachy person. At some point the headaches progressed to migraine. Fortunately, for most of my life I had infrequent episodic migraine (EM). An attack would start, I’d treat it with ibuprofen and I was better in an hour. I sought treatment when I began losing a few days per month to terrible attacks that didn’t respond to over-the-counter (OTC) remedies. Over time, my frequency of attacks increased and I “chronified” while under the care of my well-intentioned primary care physicians.
My goal is to help you get the frequency and duration of your attacks to back-off. I’ll help you understand the concept of chronification of migraine. Episodic migraine basics will be shared along with links for blogs that I consider required reading. A 4-step plan will help you get the relief you are looking for.
According to a prominent headache specialist, Dr. Carolyn Bernstein, a headache specialist at Brigham and Women’s Hospital, 50% of managing migraine is education. Kudos to you for being here to educate yourself. Let’s figure out your personal action plan to discover noticeable, lasting relief.
**While Migraine Strong writes about the latest in migraine treatments, this is not medical advice. We are patient educators and all information you read should be discussed with your doctor.
Differences Between Chronic and Episodic Migraine
I was diagnosed with chronic migraine (CM) after seeking help from a headache specialist. Simply put, episodic migraine is characterized by having up to 14 migraine days per month. Chronic migraine is when you have headache for 15 days or more of the month where 8 or more of the attacks meet the definition of migraine. When this occurs for 3 months or more, you meet the criteria for chronic migraine. It’s a horrendous place to be. Most of us can avoid it. In my case, I had unrelenting head pain around-the-clock for about 3 months before things started to gradually fade.
How It All Starts
Your genes are likely your root cause of migraine. Migraine brains are hyper-responsive to normal, benign, everyday stimulation. The combination of factors that triggers your headaches and migraine is unique to you. It’s worth spending some time trying to identify the set of factors that bring about your dreaded attacks.
Just because migraine is overwhelmingly due to genetics and some triggers are beyond your control, there are many ways to significantly decrease your attacks.
Required reading assignment #1 is this informative blog about The Bucket Theory. This is fundamental to understanding what contributes to headaches and migraine overall and why it can be hard to pinpoint specific triggers.
Chronification – What It Means
I haven’t checked a standard dictionary, but I doubt I’d find the word “chronification” on its pages. Migraine attacks and headaches can “chronify” when they happen more frequently over a long period of time. It seems that the structure and function of some of the neurons in the brain change and “learn pain.” The overly sensitive brain starts interpreting normal, everyday stimulation as pain. You might notice that sounds, lights and smells “hurt” when they didn’t before even if you aren’t in the middle of an attack.
During the 2018 Migraine World Summit, Dr. Alan Purdy, the president of the American Headache Society said “migraine literally just hijacks normal pathways of your brain to produce its symptomology” in chronification.
For me, my brain definitely felt hijacked when I became chronic. My ENT doctor said that my pain switch was stuck in the “on” position.” I left that appointment feeling like I hit another dead end. She used the term “runaway pain” as her hand was turning the doorknob leaving me with that awful, depressing concept and no suggestions about what to do about it.
Flipping the “switch” to the “on” position is usually avoidable
According to Dr. Robert Cowan, Director of the Division of Headache and Facial Pain at Stanford University, two risk factors for converting episodic to chronic migraine that are within our control are medication-overuse and ineffective acute treatment of headaches and migraine attacks. Let’s take a deeper look at these two controllable issues. They are only controllable when you know what gets out of control and when.
Migraine and medications
Acute medications – I have a love-hate relationship with the medications I used most often for treating my acute attacks.
My husband and I used to joke about buying stock in the company that makes Advil. Between my neck problems (herniated discs) and my head pain, I took a LOT of Advil plus a little Aleve and Excedrin Migraine. I went to my primary doctor when Advil wasn’t working as well and I was losing more and more days to the welcoming darkness and quiet of my bedroom.
My doctor prescribed sumatriptan. This was a miracle drug for me. The attack went away in 20 minutes and I felt better than I had before the attack started. I had a new love and I was never given any guidelines or warnings about medication-overuse or rebound. The community of educators are beginning to refer to it this condition as medication-adaptation headache. The word “overuse” implies that it’s the fault of the person with migraine. Since medication-adaptation headache is a mouthful, I’ll continue to use the word “rebound” for now.
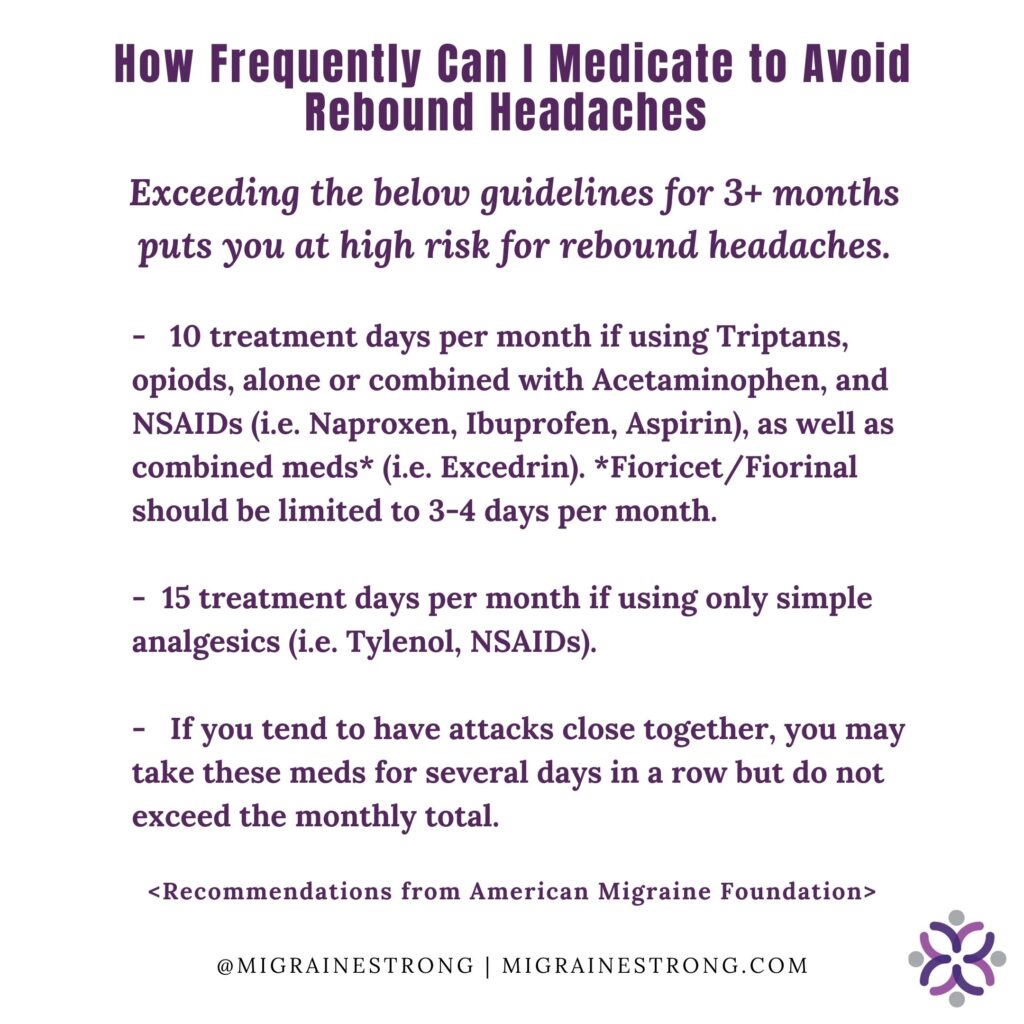
My well-meaning doctor never advised me to limit the number of treatment days each week to 2-3 and no limit was imposed by my insurance company. I did not know that we are supposed to limit treatment days to a total of 10 when using triptans and NSAIDS like Aleve, Advil and Excedrin. Between treating my neck pain and headaches with Advil or Aleve and migraine attacks with sumatriptan and Excedrin, I fell into rebound. The meds that gave me my life back ultimately hurt me as I was uninformed.
Understanding medication-overuse or rebound
To spare you from this experience, required reading assignment #2 is all about rebound / medication overuse headache. Avoiding this common pitfall is critically important.These medications can be truly wonderful when used properly. There is no need to be afraid of them. Keep reading and educate yourself about potential migraine and medication pitfalls.
Here is a handy graphic that you can download to your phone as a reminder of the limits:
Migraine medication options
Now that you are familiar with a common downside of over-the-counter and prescribed migraine medications you should know that you have quite a few choices. The most commonly prescribed medication in the class of meds called triptan is sumatriptan but there are many others. If one does not work for you, try others as they are all slightly different.
Some come in nasal sprays or injectable forms so you can still use them if you have nausea and vomiting. If you have a medical concern and cannot take a triptan, there are still several options. Some people find relief from prescribed anti-nausea meds (i.e Zofran, Compazine) and muscle relaxers. A lesser-known but excellent abortive is Timolol.
New migraine specific medications
Over the last couple of years, new migraine specific medications have come to market. Two block CGRP (calcitonin gene related peptide) which is causally linked to migraine attacks. These medications are Nurtec (also recently approved to be used preventively)and Ubrelvy. Neither of these medications will trigger a rebound effect. Being able to take them in addition to other medications like NSAIDs and triptans helps to increase the treatment days allowed and lower rebound risk. The third new medication is Reyvow which acts similarly to a triptan without the vasoconstriction of blood vessels that make triptans a non option for those with heart or stroke issues.
These new medications are expensive. The manufacturers offer patient assistance programs to help with affordability. However, these are only available for people with commercial insurance which leaves those with government insurance out of luck. Most of these meds are just under $1,000/month and that is just not an option for many who need it most.
Having a doctor that understands the many options you may have is critically important. You might have to find a headache specialist who can find the right migraine cocktail for you. With the relatively new arrival of the anti-CGRP medications, there is a lot of reason to feel hopeful.
The timing of migraine and medications
The timing and dose of acute medications is important. Typically, doctors will advise their patients to take the acute medication as soon as they notice migraine symptoms starting. So, make sure you have your meds with you. Some people find it very helpful to put together a handy migraine kit.
Regarding dose, take the full amount that your doctor prescribed. Because many of us are prescribed triptans and only have a few triptans to use each month, some people cut their pills in half. This often is not enough to knock the migraine out. Experts warn that this practice often can lead to taking more medication and rebound / medication-overuse as the attack either does not completely subside or it only subsides for a few hours.
Some doctors advise their patients to boost the effectiveness of the triptan by combining it with an NSAID like Aleve (naproxen sodium), Benadryl and a nap when practical. As always, consult your doctor before combining medications in this way. I am sharing what works for me as well as what is commonly reported by others. *This is not medical advice.*
The conundrum of when and if to treat
As I said above, doctors recommend treating migraine at the first signs for best results. This is great advice for someone with infrequent, episodic migraine attacks. But what if you are afraid of needing to medicate more often than suggested 2-3 times per week? What if you only have 6-9 tablets of prescribed medications per month and you typically have symptoms on more that 6 -9 days per month? This is quite a quandary that many of us find ourselves in.
It’s hard to know if the sensation you feel is going to be a full-blown attack. Nobody wants to run out of their precious few pills before they can get a refill. And, now that you know the risks of rebound, you want to minimize the chances of that complication. Below is a handy list of things to do before you reach for your limited migraine medication.
Our article about ginger is required reading #3. Ginger is an excellent non-pharmaceutical abortive for migraine.

Migraine medications to avoid
A few words of caution about 2 medications that were used decades ago to treat headaches and migraine; Fioricet (acetaminophen, butalbital, and caffeine) and Fiorinal (aspirin, butalbital, and caffeine). Many neurologists and doctors who specialize in headache disorders avoid prescribing them for good reason. These meds, especially when not strictly limited can cause rebound quickly, sometimes in as little as four doses a month, according to the American Migraine Foundation. If you currently take these meds, you may need a plan to find an alternative in order to get yourself better.
When to consider a preventive medication
There is a lot to consider regarding when or if a daily preventive, Botox or anti-CGRP preventive medication should be started. Before I mention some of those factors, I think a preventive strategy should always be implemented when you notice occasional attacks becoming more frequent. A preventive strategy would include trying evidence-based supplements and lifestyle changes including diet changes*, prioritizing quality sleep, increasing intentional movement and stress reduction. Migraine prevention is not just about medications.
A consideration before starting preventive medications is the degree of disability you experience each month. Getting 4 attacks per month that respond to treatment within an hour is very different from getting 4 attacks each month that are resistant to medications and leave you unable to take care of yourself and/or others.
Other factors include your age, medical history, insurance coverage, current state of wellness and co-morbidities often seen with migraine (i.e. depression and anxiety). For some women, hormone replacement therapy may be most helpful. In a situation where a person has high blood pressure, switching to a blood pressure medication that also helps migraine may be very helpful. Check out our comprehensive guide to preventive migraine medications to get a better understanding of the many options. Your healthcare team should help you understand your choices.
My own opinion about preventive medication
My personal belief is that it’s best to try the non-pharmaceutical approach first as most migraine medications have side effects and can be expensive. This is a topic for another time, but sometimes people delay medications too long and chronify. It’s harder to treat chronic migraine than episodic migraine, so I encourage you to not wait too long.
On the other hand, some people jump to medications and overlook lifestyle changes that may help them. What if you could cut the number of attacks you get in half by using natural migraine treatments that actually work and only needed acute medications once a week? It is important to state that needing to change your lifestyle does NOT mean migraine is your fault. Further, deciding to not change your lifestyle does not mean you are “bringing it on yourself.” Migraine is a genetic disease and not anyone’s fault. Do not judge decisions about lifestyle choices, yours or anyone else’s. Having migraine is enough of a stigma.
Medications taken for other health issues that may be increasing your migraine attacks
This was an eye-opening topic during the Migraine World Summit in 2018. Dr. Andrew Charles, Director of Research and Treatment at UCLA’s headache center, discussed medications that can be problematic for those of us prone to migraine. He and many on the community of migraine specialists are frustrated there is little or no research to confirm some of their observations.
Their experience has shown that the below medications are sometimes part of the problem with their patients living with migraine. He urges a careful look at the below classes of medications to see if they remain necessary for you. Migraine and medication management can be tricky. Your doctor may be able to recommend a suitable alternative. Please do not make any changes without including your doctor:
Medications to Evaluate
- SSRI anti-depressants like Prozac, Paxil and Zoloft- Anxiety and depression often occur along side migraine. The class of anti-depressant medications that may be a better alternative for people with migraine is the class called SNRIs. Example brand names are Effexor, Cymbalta and Pristiq. Make any changes with your doctor after careful consideration. We have a blog about migraine and anxiety that you may find helpful.
- Gastro-esophageal reflux medications like Nexium, Protonix, Prilosec- The class of medications called proton-pump inhibitors (PPI) serve as migraine triggers for some people. Some in the class seem to be worse than others and it’s possible that you may benefit from a change in type or a lower dosage. If your PPI is prescribed, check with your doctor to see if transitioning to a Histamine-2 blocker will be effective. An OTC example of this is Pepcid. To avoid rebound effects from discontinuing PPIs, your dose should be tapered and not abruptly stopped. Ask your doctor or pharmacist how to best taper and/or transition properly
- Nasal steroids like Flonase and Nasonex and decongestants like Claritin D- Dr. Charles acknowledged that some people have disabling allergies that need frequent or daily treatment. He encouraged people to only take these medications when truly needed and consider anti-histamines as possible alternatives. Flonase-triggered migraine attacks usually show up within 4 days of the start of use.
- Oral contraceptives and hormones for menopause– Dr. Charles discussed this at length. In summary, taking oral contraceptives may exacerbate migraine attacks or make them better. It’s important to consider these medications and their possible role in your overall approach to managing migraine attacks. Regarding hormones for menopause, many postmenopausal women take estradiol for extended periods of time. Many headache specialists believe this can also exacerbate migraine. There may be topical preparations that address symptoms of menopause rather than taking an oral hormone.
- Pain medications- Dr. Charles was clear to state that pain medications can be a particular problem for people with migraine, but that it’s not an issue of addiction or dependence. Aside from the issue with rebound, pain medications seem to make migraine worse. The mechanism isn’t known, but the theory is that certain pain medications like codeine, hydrocodone and oxycodone change the way the brain perceives pain and are harmful overall. He was very specific about potential harm from Fiorinal and Esgic/Fioricet. Dr. Charles was also specific about caffeine-containing pain meds like Excedrin Migraine worsening and/or sustaining the problem when used too often.
Your personal plan to roll-back your attacks:
What probably brought you to this part of the internet was your desire to get your increasing migraine attacks to back-off. We are glad you are here educating yourself. Now is the time to do what it takes to gradually have more symptom-free time. Put measures in place so you do not chronify. Here are 4 steps you can take to get migraine in better control.
Step 1 – Seek effective medical help.
If you have seen a general practitioner and things are not getting better after several months, seek the advice of a general neurologist or headache specialist. Preparing for your visit is important. If you don’t have access to a specialist, you can still get better but it might take more effort.
Step 2 – Track your headaches and migraine attacks
Trackers like Migraine Buddy can be very helpful. This info is vital to seeing patterns in your potential triggers as well as in treatment frequency and effectiveness. Headache specialists will be interested in seeing changes in your pattern over time. This is also a very good way of helping you describe to your doctor your degree of disability, too.
Step 3– Look at your current usage of migraine medications
Can you make it more effective after consulting with your doctor? Maybe your current plan just needs to be tweaked. If you are in rebound or at risk for it, address this right away so you do not develop chronic migraine. This blog can help you escape rebound. There are effective medication combinations that can help you during rough times without putting you in rebound.
Step 4– Consider the effect of medications you may be taking for other conditions
You may be taking medications for other conditions like GE reflux that could be adding to “your Bucket” (see required reading #1). Consider alternatives if you and your doctor believe you need continued treatment.
Migraine attacks of increasing frequency, duration and intensity can be rolled-back. Education and the right medical team are critically important. If you’d like more information about managing migraine in an upbeat, supportive community, please join us in our closed (private) Facebook group called Migraine Strong or check us out on Instagram.
* There are several dietary approaches to managing migraine. The Migraine Strong Team has written at least 6 articles about migraine-oriented eating for you to explore. Here are just 3 but we invite you to look at the others, too:
Fish Oil and Migraine-Can it Really Help?
You have shared so much helpful information here. Your two charts — Avoiding Rebound Headaches and Before You Take That (medication) — are solid gold! Everyone should print, post and circulate copies of them both.