I have always been a headachy person. Fortunately, migraine didn’t interfere with my life in a debilitating way until my 40s. Perimenopause was the culprit. Having gone through perimenopause with migraine does not make me an expert. It’s one of my areas of interest as a patient and patient advocate.
I have poured over the literature on migraine and migraines as well as watched in-depth interviews of 4 well-recognized experts in this area that were interviewed during the five Migraine World Summit broadcasts. Their intention was to help during a difficult, undiscussed time and that is my intention, too.
My Story
I hit the big menopause milestone 6 years ago. I was 48 and relieved to hit this marker as my gynecologist told me that perimenopause can last 10 years for some women. My best guess is that peri lasted about 6 years for me.
I have to say that there were Hellish times, especially when 24/7 migraine symptoms descended upon me. So, based on what I had heard, I was waiting for my migraine symptoms to dramatically fade away and let me get back to my full life. Unfortunately, that did not happen.
Here I sit, writing an article with a headache that just moved to my jaw, having a mild hot flash, craving cookies and especially short on sleep. My gynecologist was right about menopause. In addition to perimenopause often lasting up to 10 years, menopausal symptoms can continue on sporadically for 10 years or more. I just medicated for the second time this week but I’m now ready to share with you all that I can to help you navigate through migraines and menopause as best you can.
While Migraine Strong writes about the latest in migraine treatments, this is not medical advice. We are patient educators and all information you read should be discussed with your doctor.
My Goals for You
My goals are to help explain more about migraine in midlife so you can see where your approach to managing attacks may need to be tweaked or overhauled. I’ll help you understand what you can do and what you might need from your healthcare team. My intention is for you to read this and come away with at least 3 valuable nuggets of info that will help you reduce the intensity, frequency and duration of these hormonal migraine attacks.
Special thanks goes to some of the wonderful women in our Migraine Strong Facebook group who contributed to this blog by helping me understand specific questions they wanted answered. Each question was written from the perspective of a woman with known hormonal migraine seeking help and information on what to expect of migraines and menopause.
Premenopause, Menopause and Post-menopause Defined
Premenopause
Pre-menopause refers to the reproductive years before your body starts preparing for menopause, the start of your non-reproductive years. Some of you already know that your attacks are hormonal. They may be pure menstrual migraine where they only occur for a few days around your period. Or, they may be menstrual-related migraine where they typically happen around your period but also occur at other times of the month. Many women with known hormonal migraine wonder if menopause will bring relief.
Dr. Susan Hutchinson , a headache specialist and family practice physician dedicated to treating migraine, mood disorders says, “We are our hormones.” Her interview during the Migraine World Summit (MWS) in 2017 was incredibly interesting. Later in this article I will have more from this doctor who is passionate about helping women with migraines through menopause. She has even written a book about this topic.
So, What is a Hormone?
Hormones are chemical messengers made by one organ to influence another. For example, our brain makes follicle stimulating hormone (FSH) that travels to our ovaries. The FSH stimulates our ovaries to make the hormone, estrogen. Estrogen then goes to a variety of organs in our bodies and exerts its effect on them.
Perimenopause
My gynecologist told me during perimenopause our ovaries are running out of eggs and trying to go to sleep after many years of hard work. The brain senses this and keeps trying to wake them up by sending pulses of different levels of FSH to get them to make more estrogen. Eventually the ovaries go to sleep after a lot of tossing and turning even though the brain is still doing it’s best to wake them up by making a lot of FSH.
Perimenopause is a time of great change. In hushed tones, previous generations often called it “the change.” It’s certainly a time of many physical changes that often occur with other personal and emotional milestones in a woman’s life.
Unfortunately, even as open as our culture has gotten to discussing sex and money, perimenopause is rarely discussed even among women in the 40s who are in the middle of it. I remember being thrilled while at a bunco gathering with some friends when I offered to pour a glass of wine for a friend and heard her say under her breath, after a heavy sigh, “hot flash.” We both brightened and chuckled about how we were dealing with “the change.” I think she was relieved to have someone to talk with who was going through the same thing.
Menopause
Your last period is considered the start of menopause. Officially, a doctor doesn’t consider it your last period until 12 months after. That’s right, menopause is officially declared 12 months after your last period. It is one date on the calendar that you marked that is confirmed as highly relevant in a year. This is one reason why your gynecologist wants you to get especially good at tracking your period during perimenopause.
In the US, the average age of menopause is 51. So, it would not be uncommon for many women to notice perimenopausal changes as early as their mid-30s.
Post-menopause is officially the term used to refer to time in your life after that last menstrual cycle. But, we usually just call it menopause and that’s how it will be referred to in this article.
Migraines and menopause brought you to read this far so yes, increased headaches and migraine are certainly commonly reported. Hot flashes, night sweats, moodiness, depression, sleeplessness, palpitations and muscle/joint pains are all common symptoms that are frequently discussed with doctors by women in perimenopause.
Symptoms of Migraines and Menopause
To make things even more challenging for us and the doctors trying to help us, there is great overlap in the signs of aging and perimenopause and symptoms and side effects of migraine and some migraine medications. The symptoms are memory issues, word-finding speed, weight gain, hair loss/changes, headaches, sleep disturbances and mood changes. Again, keeping track of your period and symptoms can help figure things out where possible. It’s hard to tease-out exactly what is causing these frustrating and real issues.
It is beyond the scope of this article to discuss the many other changes our bodies go through in peri and menopause. This is a good overview of menopause if you wish to learn more.
How long do these phases last?
It’s not uncommon for symptoms of peri to begin 10 years before your very last period. Most resources and doctors say 4-5 years but if you have hormone-related migraine like 60% of women, and you are in your 40s, there’s a good chance you are in perimenopause.
Once in menopause our bodies continue to adjust to the naturally altered hormone levels. In menopause, you should expect less severe and frequent symptoms of fluctuating hormones, but there’s a good chance the diminishing symptoms will take significant time to fade.
Dr. Anne MacGregor was interviewed for the Migraine World Summit in 2018 and 2019. She is quite a catch for the MWS as she is a specialist in headache and women’s health and one of the world’s leading researchers in the field of hormonal effects on migraine. And, she is quite a dynamic speaker! Dr. MacGregor says some women have symptoms for another 10 years after their last period. There are women in their 80s who still get hot flashes.
What Blood Tests Tell Us
It’s important to understand that overwhelmingly, those of us that experience hormonal migraine whether it’s menstrual migraine or from perimenopause, have normal hormone levels. It’s our migraine brain that is hyper-responsive and thinks something is wrong. In a person who is not genetically predisposed to migraine, they have the same normal hormonal fluctuations and do not have headache and migraine symptoms.
Blood tests are not typically ordered by doctors as hormone levels vary by the hour, day and month. Hormones are often pulsed into the bloodsteam. The lab information doesn’t usually tell them much. Doctors typically make the determination of perimenopause and menopause by what we report.
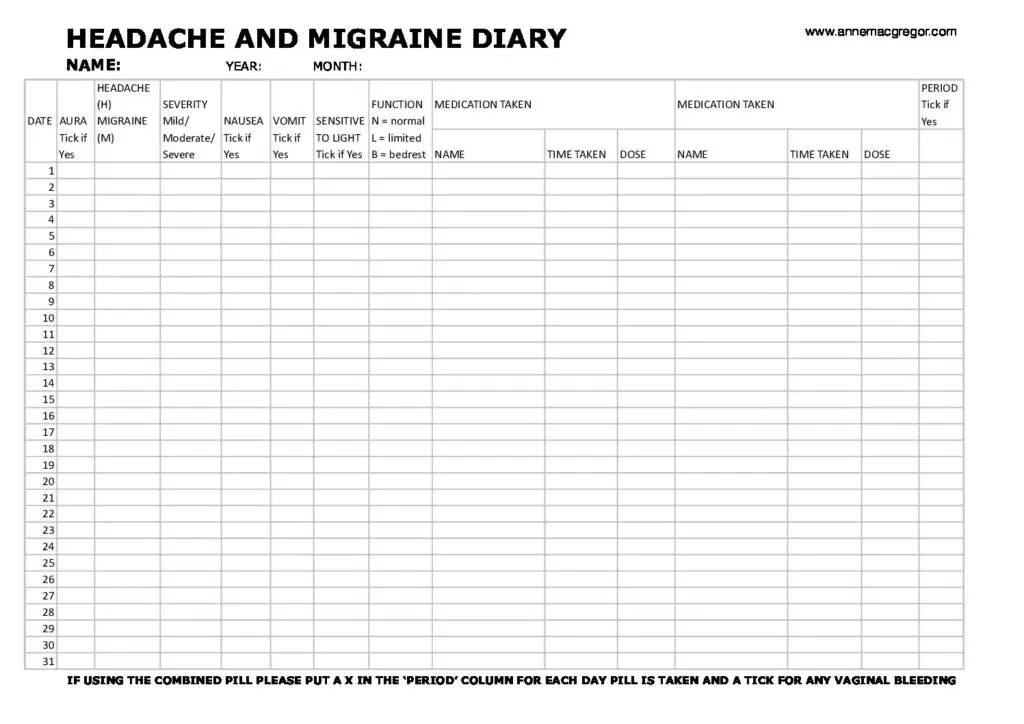
All 4 of the specialists in the Migraine World Summit (MWS) interviews were emphatic about the importance of keeping track of your menstrual cycle and symptoms of migraine as well as the usual perimenopause symptoms like night-sweats, hot flashes and altered mood. This info is very important to get the right help managing migraine and menopause.
This is the tracking form that Dr. MacGregor uses with her patients.
Can You Expect Improvement in Migraine with Menopause?
Dr. Hutchison, in the MWS for 2020 said she gets excited for the women who are really struggling during perimenopause as it shows a strong hormonal connection. This strongly suggests that menopause will bring relief. Statistics say that 2/3 of women that go through natural menopause (as opposed to surgical or chemical menopause) improve and have fewer migraines in menopause.
Some studies have shown conflicting results, but all 4 of the doctors interviewed were specialists in both migraine and women’s health and they all agreed that most women can expect significant improvement.
For those with pure menstrual migraine, meaning that they only get migraine attacks around their period, there is general agreement that the likelihood of improvement in menopause is strong since the likely trigger is hormonal fluctuation, specifically estrogen. With significantly lower and more stable estrogen, attacks should be less.
Dr. MaryAnn Mays, a headache specialist from the Cleveland Clinic who was interviewed about migraines and menopause during the MWS in 2016, noted that women who have migraine with aura are less likely to see improvement. So, if you don’t have migraine with aura, you are more likely to improve.
Personally, I have greatly benefited from menopause although it took a long while for my symptoms to fade while doing a lot of lifestyle changes. I’m having an unusual week of hormonal symptoms, but I usually only have to treat an attack every 6 weeks or so. While a little less careful with my lifestyle changes lately, I still take supplements. I am no longer on a migraine preventive medication. Also, I have migraine with aura occasionally so I may have been less hopeful that I’d see improvement after menopause, but I DID so I hope this gives you hope!
All 4 of the doctors strongly encouraged women with hormone-related migraine to get proper treatment and indicated that proper treatment in perimenopause leads to better outcomes in menopause. Their suggestions for treatment will be discussed later.
8 Reasons Why Migraine Symptoms Can be Worse in Perimenopause
It’s important to understand that migraine is genetic. You did not give yourself this debilitating condition. The below factors may be contributing to worsening migraines and menopause. In no way am I implying that you are at fault.
1. Fluctuations in hormones
This has already been covered but it’s worth stating again that there is nothing wrong with your hormones. Migraine is inherited. The migraine brain responds in an abnormal way to “normal” stimulation. The hormonal fluctuations in perimenopause are normal and healthy but they can trigger the cascade of neural activity that results in migraine for those of us who are genetically predisposed.
2. Hot flashes, night-sweats and sleep disturbances
When asked, most headache specialists will say that prioritizing consistent quality sleep is one of the most important things to do to help manage migraine. Perimenopause is a time when sleep can be very difficult for many. Many women have a terrible time getting enough sleep due to these common symptoms of perimenopause like night-sweats and poor sleep quality.
3. Mood swings, irritability, anger, crying
These emotions and the imbalance of neurotransmitters from natural aging may add to internal stress load and may increase the likelihood of a migraine attack
4. Midlife angst
Many women may become more aware of an unfulfilling career or relationship. If they have children they may be dealing with an “empty nest.” These factors may also add more internal turmoil.
5. Medications
While many medications list headache as a possible side effect, make sure you review all of your medications with your neurologist to make sure you haven’t added a potential culprit.
An example of a potential culprit is the class of medications called proton-pump inhibitors (PPIs). These are commonly taken for GI reflux by many people in midlife. Many headache specialists suspect PPIs of being migraine triggers. Examples of over-the-counter PPIs are Nexium, Prilosec and Prevacid. Protonix is a prescribed PPI.
6. Lifestyle changes
As we age we often become less active. Exercise has been shown to act as a migraine preventive. Exercise is not only important to our overall wellness, it’s important for migraine management. In addition, it’s important to look at other possible lifestyle changes that could impact migraine such as alcohol consumption and/or an increase in eating out or highly processed foods. Things that didn’t trigger you before may be triggering you now that your hormonal balance is very different.
7. Increased use of acute migraine medications
To avoid the risk of getting into trouble with rebound (medication overuse headache), acute medications must be limited. Sometimes our doctors do not tell us this and we end up making ourselves much worse. I found myself in this position and have written about it and what you can do if you think you make be taking too much medication. Being vigilant about acute medications is very important. If you are needing to medicate more than 2-3 times per week it’s time to step things up with your preventive regimen and consult your doctor.
If you have been using more, it’s not your fault. Your symptoms have increased and you need to function.
8. Heavier periods
Some women have heavier menstrual flow as well as more frequent menstruation. Since iron deficiency is a migraine trigger for some, Perimenopause can often cause you to have heavier blood flow during your period, which can lead to iron deficiency, another possible migraine trigger.
Additionally, those with heavy menstrual flow may release increased amounts of prostaglandins. These natural chemical substances are associated with pain, inflammation and blood vessel dilation.
Misdiagnosis and Underdiagnosis of Migraine
According to the American Migraine Foundation (AMF), 4 out of 5 people with chronic migraine are misdiagnosed or mistreated. One of the most frustrating complaints that we hear about in our Migraine Strong Facebook Group is that people were not properly diagnosed for many years. We frequently hear that people were told they had sinus headaches or were just stressed or anxious. According to the AMF migraine is most often misdiagnosed as a sinus headache. This comes up often when speaking with women struggling with migraines and menopause. Read our article about sinus headache if this sounds like you.
Unfortunately, migraine is a stigmatized disease and often people don’t seek treatment. The lack of self-advocacy coupled with physicians that do not recognize migraine can lead to years of unnecessary suffering.
Additionally, when migraine is not properly treated and patient, “chronification” can set in. This is from the AMF: “While the observation that migraine chronification is linked to a progressive increase in headache frequency may seem self evident, it is in line with rapidly accumulating scientific evidence that the brain “learns pain” and that early therapeutic intervention—before migraine attacks have reached a critical level of frequency—may serve to prevent the chronification process. Do not delay in seeking treatment! Recent studies have indicated that chronic migraine occurring daily for more than 6 months is particularly difficult to reverse.”
Given the fact that perimenopause lasts for years, it’s vitally important that you not delay in getting the proper help so that you avoid chronification in midlife.
Perimenopause and Vestibular Migraine
Well, my friends with vestibular migraine (VM), I got excited about finding some good data and tips specifically for you, but the connection between perimenopause and VM is scientifically unsatisfying. **Big sigh.** There is no neat and tidy data as there is not nearly enough research done on VM nor perimenopause. Suffice it to say that there is almost no published research on both VM and peri together. It seems that there is recognition by doctors who often treat VM that there is an increase in symptoms in perimenopause but little data.
Dr. Timothy Hain, one of the most prestigious VM doctors wrote about migraine headache in menopause. What is striking is that in his “dizzy practice,” most of his patients are about 50 years old whereas the peak age for migraine in the general population is about 35 years old. As said earlier, the average age of menopause is 51.
Personally, I do not have VM but I had a lot of vestibular symptoms when I was in perimenopause. Now that I am in menopause but going through another surge in hormonal symptoms, I also have more vestibular symptoms. Me thinks there’s a link.
Treating Migraines and Menopause
All 4 of these wonderful, dedicated doctors interviewed for the 5 Migraine World Summits were emphatic and in unison about quite a few things. These 4 treatments may be critical to helping those of you trying to understand what you can do NOW whether you are pre-menopausal, perimenopausal or menopausal.
1. Find the Experts
Seek a doctor with expertise in BOTH treating migraines and menopause. This may be a tall order for many of you. Perimenopause and migraine can be a double-whammy in terms of getting the right kind of help from our healthcare providers. Primary care doctors refer you to your gyn for help but your gyn refers you to your neurologist who refers you back to your gyn. Who the heck can help us? For some people, seeing a board certified headache specialist may not even be possible.
Dr. Hutchinson not only makes sure she sees her perimenopausal patients every 2-3 months, they have her email so they can stay in touch and keep a thoughtful, dynamic relationship in place.
In this article about what to do if you cannot see a specialist you will find excellent ideas that apply to the dilemma of not having a doctor that is comfortable with treating the combined double-whammy of migraine and hormones. More work is required on your part but the pay-off is likely worth it.
While not experts in migraine, there are doctors who specialize in menopause who might be excellent resources for you. Improving peri and menopause symptoms may also bring migraine symptoms in better control.
2. Bioidentical hormones and migraine
Hormone replacement therapy (HRT). Yes, this is a controversial topic. In her talk, Dr. MacGregor specifically discusses the controversy and what has been learned. She believes it was once overused and wrongly used and is now not used enough and properly to really help women who are struggling with migraine ad menopause. Much of the published literature uses older medications and outdated practices. Things are much different now.
According to Dr. MacGregor, estrogen is given in a safer way now through a patch or gel that is rubbed in. While in perimenopause there is a lot of fluctuation of estrogen. When steady amounts of estrogen are given transdermally, the natural fluctuation that was causing trouble starts to level-off and the symptoms lessen.
She advocates bioidentical hormones for migraine. They are plant-sourced but identical and indistinguishable from estrogen made by a woman’s body. When using estrogen in someone with a uterus, progesterone is also prescribed. Without the progesterone, the lining of the uterus may get too thick and cause serious problems with the uterine lining like cancer.
MacGregor went on to discuss risks. When therapy is timed properly in peri, there is a very slight increase in breast CA when using estrogen and progesterone together. The risk goes away with estrogen-only treatment but that is only appropriate for women without a uterus. There may be protection from breast CA in estrogen-only HRT for those who have had a hysterectomy. The risk happens with the wrong kind of therapy.
I was shocked to hear a statistic that Dr. Macgregor shared. She said that HRT is 90% effective for managing menopause symptoms and quite high for migraine in perimenopause. Based on that number, bioidentical hormones and migraine is certainly worth some further exploration even though it has not caught on in many areas of the US.
Helpful Resources
Another wonderful resource comes from Dr Louise Newson, a British general practitioner and menopause specialist who also has migraine. She echos much of what Dr. MacGregor says and seems equally as passionate about getting the word out and helping women with migraine and menopause. This Youtube video about migraine and menopause answers many questions specifically about bioidentical hormones and migraine relief.
Dr. Newson and Dr. Sarah Ball, menopause specialist, have their top tips complied here for managing menopause and migraine.
Dr. Judith Pearson, a specialist from the National Migraine Centre in London compiled this nice handout that is packed with excellent information on Hormonal Headaches and the Perimenopause
Antidepressants
“Estrogen is associated with increased production of serotonin, reduced serotonin reuptake, and decreased serotonin degradation. The consequent cyclical changes in serotonin levels in trigeminal ganglia could contribute to the selective response to estrogen withdrawal.” This is a technical way of saying that changing levels of estrogen can and do change the levels of another hormone (serotonin) that can effect an important part of the migraine cascade. So, logically you would think that helping serotonin to stay steadier would help migraine. It turns out that is does.
Both Dr. MacGregor and Dr. Hutchinson discussed the important role that 2 classes of antidepressants can play for us.
SSRIs
The drug class called selective serotonin uptake inhibitors (SSRIs) are commonly prescribed for anxiety, depression and the well-known and common symptoms of menopause, hot flashes, night sweats and sleeplessness. The common brand names are Zoloft, Prozac and Lexapro.
Serotonin is known as a “happiness hormone” as helps regulate mood and is helpful for the positive feelings like pleasure and joy.
SNRIs
Another class of antideprensants, serotonin-norepinephrine reuptake inhibitors (SNRIs) impact levels of both serotonin and norepinephrine and are commonly prescribed for some of the same conditions treated by SSRIs. Dr. Hain often recommends the SNRI, venlafaxine (Effexor), in his “dizzy clinic” for his migraine and vestibular migraine patients especially when they have hot flashes as he finds it very effective.
According to Dr. MacGregor SSRIs and SNRIs are effective although not as effective as HRT. Whereas HRT is ~90% effective on menopausal symptoms, the antidepressants are ~50% effective. Not bad!
Since many physicians are not comfortable prescribing HRT and some people with migraine may be uncomfortable with any increased risk of clotting/stroke or breast cancer, SSRIs or SNRIs may be an excellent option to help reduce both menopause symptoms as well and migraine.
3. Migraine medications
While HRT and antidepressants are specific for help with migraine and menopause, there are many options to work through with your healthcare providers. There are quite a few new medications that may help you with acute treatments and prevention of attacks
Here is an up-to-diet guide on acute medications that you can learn from and ask your doctors about. Perhaps pre-emptive triptans can help you. There are 7 different triptans. It’s not uncommon to the first 2 or 3 varieties to not work. Keep trying! If triptans are not an option for you there are quite a few other approaches.
Menstrual migraine is considered more resistant and difficult to treat but there are many success stories. You can be a success story but you must be willing to keep trying. You might only be able to turn-down the intensity and/or duration but it’s worth continuing and stayoing open to new approaches.
In the coming weeks we will publish a comprehensive guide to preventive treatments that might be just the thing to help you and your doctor find the best way to minimize your uptick in hormonal migraine attacks.
What About Hysterectomy for Migraine Relief?
According to Dr. MacGregor,“hysterectomy is probably the most inappropriate management of menstrual migraine.” Her opinion as well as the other 3 doctors interviewed for the MWS is that hysterectomy is not an appropriate strategy. She acknowledges that there are no published studies of hysterectomy followed by bioidentical hormones and migraine but firmly believes there are better strategies and that women should keep their reproductive organs when medically possible.
When Effective Treatments Stop Working
This is commonly discussed with specialists as girls and women go through many physical changes through their lives. Dr. Allan Purdy, an esteemed headache specialist was interviewed about migraine and aging during the Migraine World Summit in 2018. He detailed how the body changes and why certain medications and interventions may stop working during different stages of life.
It’s important to note that as people age and develop other medical conditions, certain treatments often need to be changed. Additionally, the elderly metabolize medications different from younger people. During the MWS in 2020, Dr. Jessica Ailani, a specialist in both headache medicine and women’s health spoke at length about how hormones change and how treatment should change through life during. She specifically spoke about women in menopausal years and her frequent advice to try different devices like neuromodulation rather than adding more oral medications. This may also be a good time to try narrow-band green light therapy like the Allay Lamp.
In light of the fact that blood pressure tends to increase with age, for those of us who have not been able to try beta-blockers, a common migraine preventive that sometimes decreases blood pressure too much, this class of medications may now be an option.
What About Those Who Worsen After Menopause?
This is another area with little published data. While there is no good time to have debilitating migraine, I’m sure it’s especially frustrating when we are usually told things get better in the menopause years.
It seems that there are a few factors that influence whether or not migraine tends to improve. Being clinically depressed is associated with worsening migraine. Having high-frequency episodic migraine or chronic migraine is also less associated with improvement. Taking pain-relief medications during perimenopause and menopause for the aches and pains of aging and getting into rebound (medication-overuse headache) may lead to worsening migraine. Also, those who seem to be less likely to improve after menopause are women who have their ovaries removed or “induced menopause.”
HRT seems to be less successful and less appropriate for women after menopause but it may be an option for you. While the 4 doctors did not lay-out a different approach for those women not helped by having lower and more steady estrogen levels, they were still very encouraging about available treatments. They were emphatic about being more aggressive about lifestyle and medical approaches to minimize attacks. If you aren’t getting better you must advocate for yourself and find a better approach.
Menopause Headaches and Natural Remedies
According to Dr. Hutchinson, “Lifestyle is HUGE!” This was said emphatically by this expert as well as the other 3 doctors. Discussions of lifestyle all centered around prioritizing sleep, learning how to handle stress better, eating a diet that was wholesome and not filled with highly processed foods and exercising.
The Treatment Pie
Migraine Strong has long advocated the importance of the Treatment Pie so it was gratifying to hear all four of the experts enthusiastically support this concept. Migraine is complex and a multi-modal approach is what helps best.
Therapy
Dr. Hutchinson also spoke about the importance of dealing with trauma and emotional turmoil from the past. She encourages therapy to help resolve past and current conflict that may be making matters worse.
Diet
During perimenopause my body changed in the worst way – foods I had grown up with as well as food that I had acquired a taste for and cooked or ordered all the time were no longer my friends. How could this be?? In my world, nearly every meal had lots of rich-tasting, fermented or aged foods. Soup wasn’t soup without a load of Parmesan cheese. What about Asian food? When I was single and living in Manhattan I had some type of Asian cuisine several nights a week. How could I not be able to eat them in my 40s? It defied logic to me. Fortunately/unfortunately it was true.
I couldn’t eat my favorite foods for quite a long time. The good news is that I can eat those foods again now that I am in menopause. My theory of why this happened relates to The Bucket Theory that was mentioned earlier. The hormonal upheaval added so much to “my bucket,” that it was constantly overflowing. Had I learned about a migraine-oriented elimination diet and had this wonderful resource from The Dizzy Cook and her book I would not have lost so many months of my life to migraine attacks.
Caffeine can be friend or foe so it is important to figure that out.
Alcohol is a common migraine trigger. You might find that it’s an even worse problem as you deal with migraines and menopause. The wine you used to enjoy may now be a problem.
External Triggers
A significant portion of Dr. Maryann Mays talk during the MWS centered around the value of determining external triggers so they could be avoided. While this sounds obvious, it’s common the hear people say, “I have no idea what triggers me.”
The list of common external triggers include: stress, lighting, scents, excessive heat, noise, diet, medications and certain movement for those with vestibular migraine.
Exercise
Did you know that exercise is considered part of migraine prevention? Being active is especially important as we age.
Prioritize Sleep
This is not easy for many in perimenopause and menopause. Poor sleep in general and night-sweats are common in midlife and after. HRT and low doses of antidepressants often help in addition to the lifestyle interventions mentioned.
These 2 blogs specific to helping people with migraine sleep better are must-reads.
Supplements for Migraine and Menopause
There are 5 nutrients with enough supporting evidence in helping migraine to recommend. However, there is not enough research behind supplements for menopause for me to feel comfortable promoting its use. This study of black cohosh showed that it was helpful in reducing hot flashes but there was no control group. Given that hormonal symptoms wax and wane over weeks, it’s hard to draw conclusions without comparison.
Handle Stress Better
For some of us, this is a skill we have never mastered. Now is the time. Perhaps you need more self-care and “me time.” If you think you would benefit from professional help, make an appointment today.
In the coming weeks, we are set to publish an article dedicated to natural treatments for migraine that will surely help you in addition to the above. Be sure to check back with us.
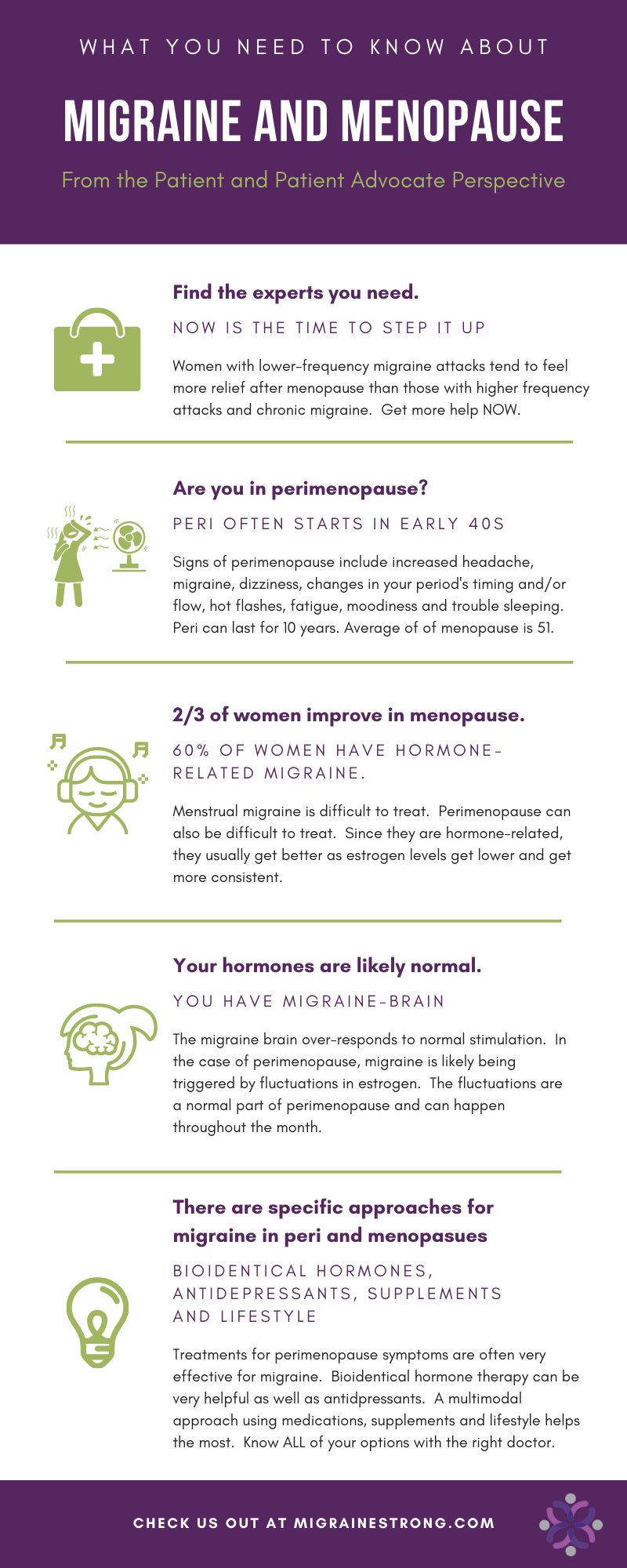
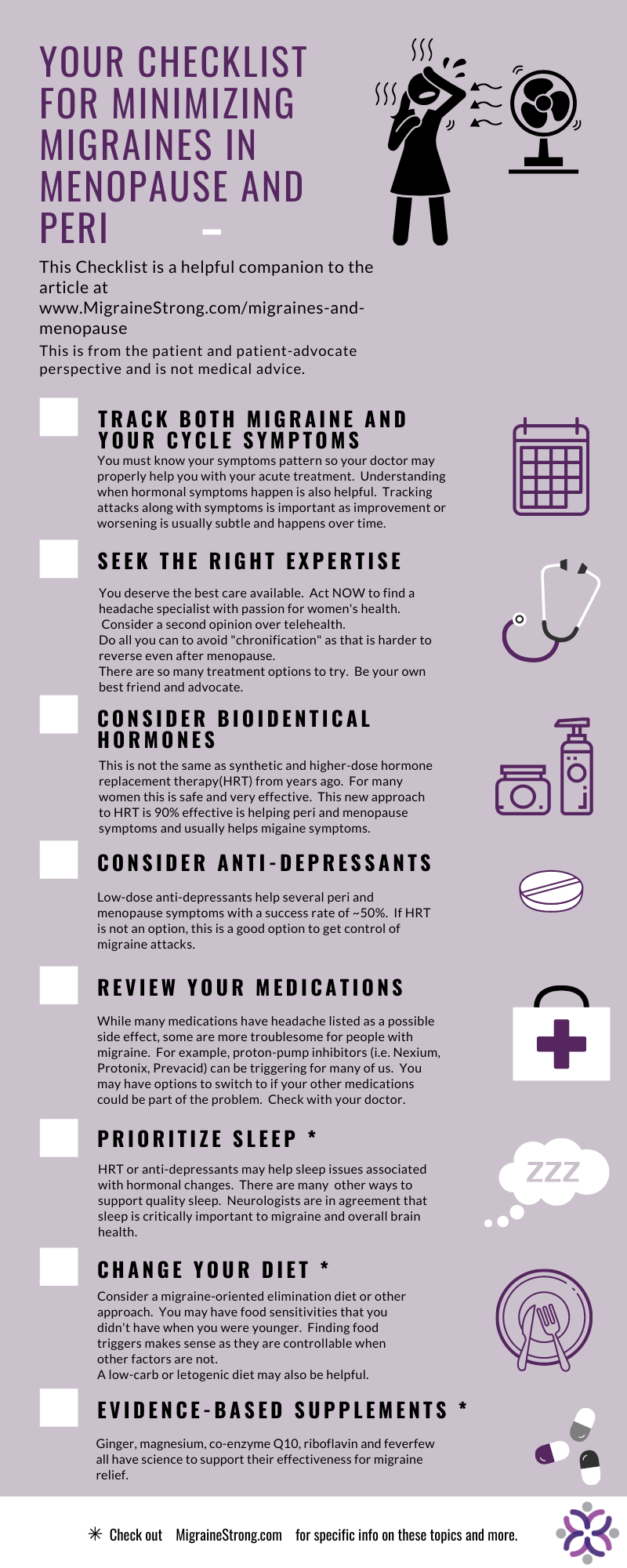
Your Checklist and Key Points
What brought you to this blog was likely either an uptick in migraine attacks, a concern of future increased attacks in midlife or information about expectations in midlife and later. My goal was for you to come away with at least 3 take-away ideas that you can either implement on your own or consult your healthcare providers about to minimize migraines in menopause. I will list a few
- Track your migraine attacks so you know for sure if things are getting better or worse
- Track your cycles so you can share this with a doctor that can help you fine-tune your treatment plan
- If you are in your 40s and having more migraine attacks, you are probably in perimenopause. An uptick in attacks during mid-30s could also be triggered by perimenopause.
- There’s nothing wrong with our hormones. Our migraine brain just doesn’t like change.
- Step it up! If your doctor is not partnering with you get a second opinion or switch doctors. If you have a general neurologist, consider a headache specialist. Be your own advocate.
- Consider hormone therapy (HRT)
- Consider anti-depressants
- Consider consulting with a doctor who specializes in menopause
- Get working on a few slices of The Treatment Pie
- Consider seeking professional help for coping skills
- Make a plan for intentional, daily activity or exercise
- Try evidenced-based supplements for migraine relief
Please download these graphics to remind yourself of some key points as well as a checklist for you to consider and review with your healthcare team.
Dear Danielle.
I much appreciated your time and effort into writing this up. Anything that supports me to feel a little more “normal” is such a positive outcome. It’s not something that has been much discussed over my life time and so has been somewhat of a secret of the put up with it and get on with life.
Many thanks
Jennifer.
Thanks for taking the time to write, Jennifer. Between the stigma of migraine and the lack of discussion and social support for some rough times that some women have in perimenopause, mid-life can be harder than we expect. I hope you find some helpful interventions and feel better and better each month. – Danielle
Thank you so much for this message. I’m able to try HRT and everything else you have suggested for perimenopause migraines. I feel lucky that I only just started having them six months ago, but I’m five years into perimenopause. Other than my migraines I’m very healthy and active. I feel blessed this is all I have to deal with and that I have a wonderful PCP that listens and hears me. Thank you for the information.
We are so glad you appreciate the info. Thank you for reading the article and taking the time to send us a comment. I hope you get better and better. – Danielle
Great article thank you. I’m a vestibular migraine sufferer and have been for 14 years. Symptoms have increased dramatically over the past 3 months. While you didn’t have much to share I just want to say thank you for including us. Most people with migraine don’t know that VM exists and it gets lonely. My perimenopause journey is just starting and should prove interesting to say the least.
It’s so frustrating! VM can be very lonely but we hope we are bringing more awareness to it. I hope it gets easier for you very soon. -Danielle
What a great article. I need some advice. I have 24/7 visual disturbances, aura like symptoms and weird head sensations, memory issues and brain fog. I have had aura migraines from the time I was in puberty. In my 30’s my hormones changed and I developed vestibular migraines and no doctor who had any idea and by that time my aura migraine attacks lessend. I also have a condition called visual snow and tinnitus. The vm attacks has gotten better over time ( maybe the hormones helped me with that) but now I have 24/7 aura like symptoms, visual disturbances, visual snow, light/sound/smell sensitivity, brain fog and memory problems…Continious migraine symptoms without the headache. Every year in premenopause my migraines changed and now in menopause with a higher dose estrogen my visual disturbances gets worser and also the other symptoms, these symptoms never go away ( I have early menopause and I need my hormones)
Last year I asked advice via email from Anne macGreghor (I come from the Netherlands) and she told me it is very unlikely if hormonal changes were the primary factor because of the frequency of my symptoms. Typical migraines does not result in daily symptom she said; I have daily symptoms 24/7? Now she is saying what I have is not migraines and she has a lot of knowledge, am I right? Suggestions are welcome…I am 43 and postmenopausal for a few years. I really have no idea what to do now. I know menopause and the hrt is having a huge effect on my symptoms. My premenopause was severe with a lot of symptoms that started in my early 30’s. Thank you.
Hello and thank you for your kind words. I am impressed that Dr. MacGregor gave you some valuable feedback. Based on what you shared, I would guess that she thinks that you do not have migraine and that a doctor should pursue other possible headache disorders or secondary reasons for your symptoms. Perhaps there is a major headache center you cold travel to? – Danielle
Thank you for your answer. I send her an email so it was a short reaction. I know my migraines are hormone related because there is a pattern in it. Two years with vestibular migraines during menopause and if I change my hrt than I get migraine attacks without headache ( aura migraines) and I have persistent aura’s without headache and this also get worser when I change my hrt so it is hormone related. My gynecologist thinks migraines with headaches is menstrual migraines and that should go away with menopause. The declining hormone levels after menopause triggered vestibular migraines, tinnitus, light/sound/smell sensitivity and every hormonal adjustment has an effect on it. The worst vestibular migraines are luckily over but my head is always feeling strange.
During puberty I developed classical migraines and this pattern changed during premenopause. Classical migraines got better with less attacks but instead the vestibulair migraines came but no doctor who sees a hormonal connection and listens to me when I tell them the hrt I take has an affect. I need my hormones because of my age. I wish doctors would listen to us women because we know our own body.
Thank you for all this information. I am going to bookmark a lot of the links and really digest it over the next few days. I have dealt with menstrual migraines my whole adult life. They have become worse over the past 10 years (I am 49) and two years ago I got the added bonus of a vestibular migraine diagnosis (which is now somewhat controlled with diet and supplements). I have tried everything under the sun to deal with the monthly rollercoaster. It was a bit easier when my cycle was regular. Now it is all over the place and impossible to track. My PCP is wonderful and really is trying to work with me, but I feel whatever we try just doesn’t work long term. It’s easy to get discouraged.
It was like a lightbulb went off when you said that it’s not my hormones that are out of whack, but my brain’s sensitivity to them. I am a highly sensitive person (sounds, smells, pain, lights) so this makes sense. I did not have a single migraine while I was pregnant or nursing either of my kids so I am holding out hope that menopause is around the corner and will provide the relief I am looking for.
Do you know of any list of qualified providers who deal with both migraine and menopause?
Thanks again. 🙂
Hi Laura-
Thanks for your kind words and taking the time to write. I don’t know of any doctors that might be able to help you besides the ones mentioned in the article. If you aren’t currently seeing a doctor specializing in headache medicine or neuro-otology, that may be helpful for you. I’d make sure you aske them specifically about what you can do regarding your hormones. Perhaps HRT is an option and/or SSRIs. Good luck to you! -Danielle
This article confirms my suspicions of complex headache versus classic migraine diagnosis that I have. Menopausal, vestibular, sinus symptoms, lack of adequate diet, lack of care and poor diet choices, I see all of these symptoms in myself. I have tried SSRIs, I take a PPI, beta blockers lower my heart rate too much. Per some recommendations from your doctor sources I feel like I have a better starting point to getting my life under control. Thank you.