Migraine disease (MD) occurs on a spectrum, so much so that even people within the same family, with the same genes experience a very different variety and severity of migraine symptoms. Dr. Michael Teixido who is an otolaryngologist with a special interest in advancing the study of conditions that affect hearing and balance, says dizziness and vertigo symptoms occur in about 25% of migraine patients. That breaks down to about 3 in 100 people. Yet, in my primary care physician’s office, I am her only patient diagnosed with vestibular migraine (VM) and I live in a very densely populated county in Florida. For me this points to a problem of vestibular migraine being under recognized, under diagnosed and under treated. Follow me as I discuss the similarities of both Vestibular migraine and Meniere’s disease in hopes to arm you with the information you’ll need to find your best symptom control.
** While Migraine Strong writes about the latest in migraine treatments, this is not medical advice. We are patient educators and all information you read should be discussed with your doctor.
Vestibular Migraine Explained
A Bit About Vestibular Migraine Physiology and Dysfunction
Put simply, vestibular migraine generally refers to dizziness or vertigo that is caused by migraine. Our inner ear has five distinct vestibular organs. The utricle, saccule, and the three semicircular canals. Each one senses movement and works together to send messages to the brain so when our head moves, without thinking, we remain oriented in space. The utricle and the saccule respond to acceleration in a straight line…forward and backward, side to side and up and down and the semicircular canals sense rotational movement. Vestibular migraine is caused by migraine’s interference in this delicate motion sensing organ system. When the utricle and saccule are affected, a person may feel drop attacks, bouncing or rocking and swaying. When the semicircular canals are affected a person may feel rotational vertigo.
If you think of migraine like an electrical storm in the brain. As that storm spreads out it can affect many areas of the brain causing serious symptoms. Vestibular symptoms can result from migraine’s interference in the cortex of the brain (central dizziness), the brain stem (central dizziness) or in the inner ear itself (peripheral dizziness) and the result of interfering with our motion sensing system is faulty sensory integration. Remember my Drowning in Symptoms story where I wrote about feeling like my senses weren’t working together, ever? Well, they weren’t and neither are yours.
Triggers and Symptoms of Vestibular Migraine
Migraine attacks can happen spontaneously coming out of nowhere or they can occur as a result of interaction with specific migraine triggers. Migraine triggers generally fall into 3 categories: physiological (like hormones), environmental (like weather, fragrance or chemicals) and dietary (like histamine, monosodium glutamate and tyramine). People with vestibular migraine can experience attacks resulting from exposure to triggers in any category. This makes life very unpredictable and often challenging for those with VM because triggers affect the five organs that make VMers sensitive to movement (especially head movement) and movement really cannot be avoided.
Vestibular migraine symptoms like dizziness, vertigo, ear pressure and tinnitus are often confused with other common inner ear conditions such as Benign Paroxysmal Positional Vertigo (BPPV) or Meniere’s Disease and for very good reason. Vestibular disease symptoms are nearly exactly the same in each condition making diagnosis muddy and VM is commonly comorbid with other vestibular disease. In many instances, symptoms are exactly the same, just the pathology differs. For example, when someone has BPPV, they feel room spinning vertigo when they roll over in bed because loose crystals in the inner ear fall giving them a sensation of whirling.
A person with VM may experience vertigo when turning over in bed as well, but only because they are very sensitive to head movements which can cause that same whirling sensation. If that’s not muddy enough, VMers are more likely to experience BPPV. Approximately 22% of those with VM ALSO have comorbid BPPV!
Meniere’s Disease Explained
Possible Causes of Meniere’s Disease
Meniere’s Disease is a collection of inner ear symptoms of unknown cause making the more proper term Meniere’s Syndrome. I’ll use both terms interchangeably throughout this article for the sake of semantics. It is associated with a fluctuating collection of fluid in the inner ear, right where those 5 balance organs I mentioned earlier are located. Current thought is that Meniere’s Syndrome is actually caused by a number of possibilities. For instance, some may have a genetic predisposition or had prolonged exposure to ototoxic drugs causing inner ear harm. Others may have experienced a head trauma or contracted a viral or fungal infection of the inner ear causing injury. While others experience inner ear damage from repeated migraine attacks. The most current line of thinking is that MD is caused by an autoimmune inner ear disease or allergy.
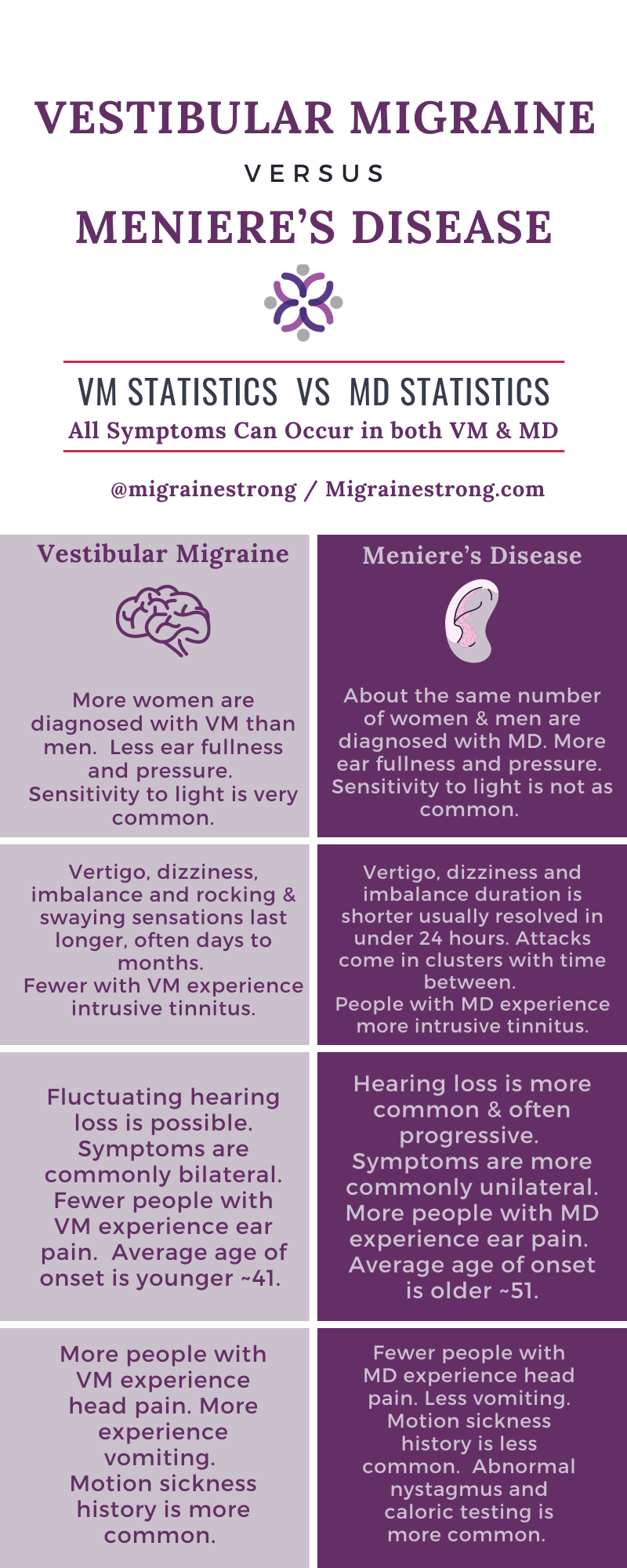
A controversial theory
One controversial theory states those with MD have an inflamed endolymphatic sac that leaks fluid into the inner ear causing attacks. MD attacks include severe spinning vertigo, ear fullness or pressure, fluctuating hearing loss (usually low frequency) and roaring tinnitus that usually last 2-4 hours followed by extreme fatigue. Men used to be diagnosed with Meniere’s Disease more often than women, but in recent years more women are being diagnosed than men. MD typically affects just one ear but it progresses, so after 30 years it affects both ears in about 50% of patients. Still even once bilateral, one ear is usually more severe than the other.
Because the ears are faulty, visual dependency is common in those with Meniere’s disease (and vestibular migraine) which results in increased sensitivity to visual movement. Our brains learn to compensate for our faulty ears (injured motion sensing organs) by depending on our eyes to determine where we are in space rather than the communication between our ears and our brain. This is why symptoms are more prevalent when it’s dark and why we are so sensitive to visual movement.
MD attacks usually occur in clusters with breaks in between. The fluid leaking theory is controversial because, not everyone with endolymphatic hydrops has MD and not everyone with MD has endolymphatic hydrops. Logically there must be more involved in the cause of MD symptoms than hydrops. As I mentioned earlier, new thought points to an autoimmune ear disease or allergy affecting the function of the endolymphatic sac in the inner ear making hydrops more of a symptom than a cause.
Similarities Between Vestibular Migraine and Meniere’s Disease
There are so many similarities between vestibular migraine and Meniere’s Disease. Just like VM, MD also seems to occur on a spectrum of severity. About 1 in 2000 people are diagnosed with MD. I’ve also seen statistics stating 1 in 1000. Either way it’s much less common than VM’s 3 in 100. Oddly MD also seems to be provoked by the same three categories of triggers mentioned above although MD patients seem to be more sensitive to salt and to MSG. Both conditions currently have no cure, but there is much a patient can do in an effort to control symptoms.
When You Have Both VM and MD
In some cases, the similarity in symptoms between vestibular migraine and Meniere’s disease may be indistinguishable. For those diagnosed with VM, about a quarter have symptoms that could meet criteria for either disease. Like many others, I have symptoms that meet the criteria for both diseases and I’ve been diagnosed with both.
Interestingly, those with MD are twice as likely to have migraine and those with migraine are more likely to have earlier onset and bilateral hearing loss from MD. Clearly migraine is very often a common thread between vestibular migraine and Meniere’s Disease. There are no specific diagnostic tests to determine vestibular migraine or Meniere’s disease. Both are currently diagnosed by excluding other disease by reviewing a patient’s personal symptom history. The inability to determine pathology is really what determines diagnosis.
While tests do exist to give clues and can strongly suggest migraine’s and/or Meniere’s disease presence, they can’t definitively determine it.
Differences Between Vestibular Migraine and Meniere’s Disease
VM is not associated with fluid in the inner ear yet many VM patients complain about the very same feelings of vertigo, tinnitus, fluctuating hearing loss and ear fullness or pressure in the ear. One marked difference is with VM, symptoms are commonly felt in both ears and attacks last much longer than MD attacks. Overall imbalance can last days to months even after spinning vertigo stops. The ear pressure VMers feel is not due to fluid like in MD. Instead, it’s the result of migraine and is similar to the sinus pressure many with more typical migraine feel in sinus cavities around their nose and eyes.
So, these inner ear symptoms MD and VMers feel might just be the way any ear behaves when its repeatedly injured and cannot recover regardless of the cause of injury. This leaves me wondering if the reason pathology is undetermined in MD is because Meniere’s Disease is very simply an injured ear?
To complicate things further…
Some research suggests repeated harm to the inner ear (peripheral vestibular system) may be projected in the brain (central nervous system) resulting in VM. Vestibular migraine is documented as being triggered after chemical ablation of the vestibular system with gentamycin injections in several patients with migraine history (but not in those without). This also suggests that injury to the peripheral vestibular system (ears) may be projected centrally (brain). These similarities point to an intimate relationship between vestibular migraine and Meniere’s disease and make for a very muddy diagnosis even for the best specialists. There is so much more research to be done.
Here’s the most interesting part:
Many patients with symptoms of both vestibular migraine and Meniere’s disease improve with migraine treatment. This is such an important piece of information for anyone reading this with symptoms of both diseases. Because migraine treatment is generally safer than MD treatment it means that in many cases, maybe migraine treatment should be considered before destructive meniere’s disease treatments like gentamycin or labrinthectomy are considered. You can hear Dr. Beh talk about migraine treatment helping a classic Meniere’s disease patient who had already had her vestibular nerve severed around minute 10 in this interview by my friend The Dizzy Cook. Dr. Teixido also mentions migraine treatment helping MD patients in his interview by The Migraine World Summit.
As I mentioned earlier VM occurs in approximately 3 of every 100 people and MD occurs in approximately 1 in 1000 or 1 in 2000 people (depending on the research you read). Yet, when I asked my doctor about her patient population she has many patients diagnosed with MD and i’m her only patient diagnosed with VM. I’d be interested to hear the results if you ask your primary care doctor the same question. I believe vestibular migraine is being under treated! And since MANY Meniere’s disease patients with vestibular migraine respond well to migraine treatment, I think seeking treatment for it is an important consideration to discuss with your doctor.
More questions than answers
A diagnosis of Meniere’s Syndrome definitely brings more questions than answers with it. If you’ve been diagnosed with Meniere’s Disease, please know my intention is not to create more questions for you. I am NOT saying that the you really have Vestibular migraine. What I am saying is there seems to be a relationship between these two diseases. So much so that some doctors believe they’re different manifestations of the same disease. Other specialists don’t buy that theory. Still, because of this connection, if you have symptoms of both diseases, you may benefit and improve your symptoms with migraine treatment.
Having both conditions myself, I rely almost entirely on VM treatment for control over my symptoms of both conditions. The only difference in my treatment from those with only VM is that I also follow a Meniere’s disease diet and I have meds on hand like methazolimide to help relieve ear pressure although I almost never have to reach for it.
So what is migraine treatment?
Many people with vestibular migraine have frequent symptoms lasting more than 15 days a month. For those people, a vestibular migraine preventative medication can be very effective. Possible medicinal treatments include sodium channel blocking drugs, beta blockers, SNRI or tricyclic anti-depressants and anti-anxiety drugs such as benzodiazepines. These medications help to calm and stabilize the brain and raise the migraine attack threshold as a result. These brain-calming medicines may also ease MD symptoms.
Because both diseases are affected by triggers, lifestyle changes recommended for migraine such as regulated sleep, hydration, exercise, trigger avoidance and stress management can be helpful in controlling symptoms for MD too. Be sure not to exercise to the point of provoking symptoms though. Exercise should be gentle and slow. Remember those with vestibular issues are very sensitive to head movement so provoking symptoms can result in a step back. If exercise makes you dizzier, be sure you return to baseline within a few minutes after exercise is complete. If it takes longer, you’re pushing too hard.
Stress management can include cognitive behavioral therapy, meditation, yoga, spending time in nature, painting and more. For more information on treatment, consider joining the Facebook group Migraine Strong.

Since dizziness and vertigo are hands down the most debilitating and difficult symptoms to deal with, my next article will focus on dizziness treatment strategies. Because vestibular disorders require a difficult and muddy diagnosis. I strongly encourage all dizzy patients to see a qualified otoneurologist or neurotologist. They are experienced in recognizing and weeding through the difference between these very similar vestibular diseases. They will help correctly diagnose and implement an effective treatment plan.
Once a proper diagnosis is in place, if VM is present, consider making an appointment with a neurologist to implement treatments that neurotologists can’t do such as botox injections or nerve blocks. This is especially important if head pain comes with your attacks. Like Neurotologists, Neurologists are AMAZING and can help tremendously with symptom control.
I hold a degree in speech language pathology and spent some time studying the ear and diseases that affect it, but this article was written from my perspective as a patient diagnosed with both vestibular migraine and Meniere’s disease. Current research was difficult to find. Therefore this article is not meant as medical advice. Your doctor will always be your best resource for that. To write this blog I relied heavily on a talk given by Dr. Texiedo at the 2018 Migraine World Summit, an article written by Dr. Hain defining Ménière’s Disease along with a study published by The National Institute of Health. You can find details about statistics listed in the chart above there. You can find Dr. Texiedo’s interview from The Migraine World Summit on his website at entad.org. Dr. Hain’s Meniere’s Disease article contains the most recent information I found and is available on his website along with a wealth of information on Vestibular Migraine, Meniere’s Disease and other vestibular disorders.
I suffered badly with meniere’s for years, had a op to releave the pressure and gradually got bit better, but in later years inbalance and eye problems got a bit worse. My daughter has been diagnosed with vm and symptoms are very similar. Found this article
Very interesting.
I am a retired plumbing contractor. I originally came down with bacterial pneumonia while working. Needless to say, I was deathly ill. Just like the virus of today. When I came home from the hospital I had all these other issues including having had a stroke. I had to sell my business. Went from one doctor to another until I was diagnosed with VM.
Now with having to wear a mask and sunglasses inside big box stores you need to be careful with sight lines. I just recently had an episode in the check out line at Costco. Finally after two weeks I am good again. Spoke with my neurologist concerning mask issue and sunglasses.He agreed this could be an on going problem. As stated above you never know when vetrigo is going to strike!I have been on medication and supplements for years. Be safe and smart.
I agree Robert! I’m so happy you finally found your answer. Stores can be a tough place for many of us with vestibular disease. Hang in there and be safe as well.
Best,
Jenn
So glad to have the resources for VM and MD. I was diagnosed with VM in 2017 and struggled for 2 years trying to find the right combo of meds. Physical therapy has helped too. Now I’m being told that I could possibly have MD as well. All I have to say is I must keep my chin up and fight every day. This article has given me some excellent info! Thank you!
Hi Karen,
Thank you for your thoughtful response. I’ve been diagnosed with both as well so I totally understand your fight. I agree movement is everything and really helps vestibular patients. Hang in there and reach out anytime.
Best,
Jenn
I was just diagnosed with VM yesterday after a history of MD, but ZERO symptoms for 22 years, until the Covid jabs. That seems to have triggered something (I’m still totally pro vax but shouldn’t have had 3rd jab after just 15 weeks), and after reading your excellent article, I think I likely have both VM & MD. I have MAJOR tinnitus and muffled hearing, both of which have historically cleared up after I recover. I know that’s not typical with VM. On the other hand, I have had all kinds of eye probs recently which sounds more like VM!
I’ve been on my a*s since Oct 7 – the day of my 3rd jab; I really should have known better because I had immediate ringing & imbalance from the first 2 jabs, but in both cases, the symptoms disappeared after a few days. In the summer, I started getting all these “vestibular migraines” which sounded to me like, “Take an Imitrex, lie down and you’ll be fine.” With my 3rd jab, I felt a huge blast of ringing and imbalance – and actually almost fell – and sprinted out before they could stop me! I knew I needed to get horizontal and here I a remain…;-)
I think they need a better name than “Vestibular Migraine” because that sounds so one-off, like you should be fine after the headache is gone and that is SO VERY WRONG!
Dexamethasone has helped and I’m already following the “Meniere’s Diet”. My Dr wants me to go on Topamax, something I’m reluctant to do, but am thinking it might be a good idea as I have been unable to work or do much of anything since the 1st week of April. Maybe Topamax can get the symptoms under control and then I can go off it.
Your story is such an inspiration! Thank you so much for sharing. I feel hope for the first time since this all started. It felt like MD, but there was so much else (blurriness etc.) and now I feel like I have some answers and can’t wait to get started.
Thank you again! Happy Thanksgiving!
Judy
Hey Judy!
I’m sorry to hear of all your struggles and pain. I started taking Topamax in November and my neurologist had to increase the dosage in December. It’s helped with getting the migraines under better control and less attacks, but I’m having more issues with my ears, pressure and tinnitus, etc. I still have issues with sensitivity to lights and sounds, which also will trigger a migraine or make one worse if I’m having one. If you haven’t tried Topamax yet, I’d say it’s worth trying based on my experiences with it so far. I’m still in the process of getting evaluated and trying to get properly diagnosed as I was in a MVA, had a TBI and Post concussion syndrome, artificial disc replacement surgery in my neck, and a 2 level fusion in my lower back. My neurologist believes the MVA caused issues with my ears, vision, and things that’s mentioned in this article. I go for a hearing test on Monday then I’m suppose to see an ENT and I start Vestibular therapy in 2 weeks. So hopefully I’ll get some more answers, but after reading this article. I wonder if I’m experiencing VM and/or MD? Do you usually have to lie down so that your symptoms will improve some? It’s nice to be able to reach out to someone who can understand what you’re going through and experiencing, although I wouldn’t wish it on anyone…..that’s for sure. Some times I just feel like no one understands and I don’t like how my lifestyle has changed due to everything while waiting for answers and just to make it through another day, ya know? What is the medication Dex that you mentioned? I wish you well and prayers go out to you as you continue to go through everything that you are.
Thank you for this information. Your are a blessing.
Thank you Jay,
Wishing you well!
Best,
Jenn
Good article highlighting these two difficult conditions. I have found that excess sodium triggers an attack of Meniere’s. The key is to balance potassium intake while reducing sodium. Also, stress is a major trigger for both of these conditions. Get the stress out of your life and your health will improve. It’s all about balance 🙂
Great advice. Thanks for your thoughtful reply Pattie.
Best,
Jenn
VERY helpful article!! Thank you!! I’ve been struggling with MD for 4 years, with ongoing dizziness and was recently diagnosed with VM also. After reading this my symptoms make more sense.
I have been diagnosed with both. This was a good article. I am currently trying to figure what treatment works for VM. I have tried multiple medications and have been unable to take them. I have applied for disability as I can no longer work full time and now it seems like I am so much worse the day after I work. I think it has to do with the stress. I think I need sometime off work to try and figure out some treatment that works. Anyway your article gave me hope. Thank you
Wow! Blow me away with all the great information here broken down so we can understand. Thank you for all the time and energy put into this.
So glad you enjoyed the article Nancy!!