When doctors and people living with migraine refer to the migraine diet or migraine elimination diet, they are talking about a low tyramine diet that is also low in glutamates, caffeine and artificial sweeteners. In 2002, it was made popular in the book Heal Your Headache, The 1-2-3 Program for Taking Charge of Your Pain , by Johns Hopkins headache specialist, Dr. David Buchholz. Dr. Carol Foster made the Charleston Diet popular and also has a book about it. Both diets are similar and have been around for a long time. Countless people have been helped by these diets but they may have a downside for some.
Why am I writing about this issue? While we love the elimination diet as one tool to treat migraine, we also acknowledge it doesn’t work for everyone. We see some people staying on an elimination diet far past the time it should have helped. We all like the idea of something so easily controlled (food and drink) being a factor in managing migraine and it can be hard to let go of the control we felt we had…even if it didn’t improve our migraine.
Additionally, some people get so much better on the diet that they are afraid to “invite trouble” and move beyond the elimination phase of the diet. It’s a nice problem to have.
All three writers at Migraine Strong have been greatly helped by the migraine diet and continue to find it very useful for people with migraine. We discuss our success often, but recognize it’s also important to discuss the pros and cons of this important tool.
** While Migraine Strong writes about the latest in migraine treatments, this is not medical advice. We are patient educators and all information you read should be discussed with your doctor.
Pros and cons of the diet
The pros
A migraine elimination diet can be a game changer in terms of managing attacks. For some people with frequent or chronic migraine, the diet can allow their daily migraine medication to work more effectively so they finally can live the lives they wish. Below is just one example of a success story.
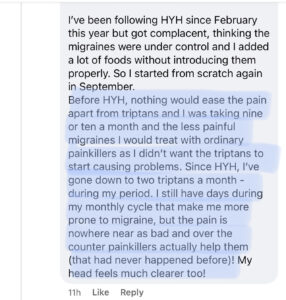
For those who wish to avoid taking a preventive or potentially stop their current preventive or minimize the need for acute migraine cocktails, diet can be a helpful tool.
Through many years of helping people though our coaching practice and social media, plus the fact that many neurologists recommend the diet to some of their patients, this intervention can play an important role.
Migraine disease occurs on a spectrum. Some people have low frequency attacks that go away with one dose of an over-the-counter (OTC) medication. Contrarily, others continue to have frequent attacks in spite of trying multiple conventional and unconventional interventions over the course of many years and many different doctors. Some will be helped by modifying their way of eating while others will have to pursue other means.
The cons
The migraine diet, even when implemented 100% for longer than intended, may not help everyone.
As stated above, many patients are advised to try the diet. It appears on the websites of some well-respected facilities that treat thousands of people with migraine like Johns Hopkins. However, some people will put off seeing a specialized doctor to try the diet before working in parallel with their doctor to coordinate an overall plan to get migraine in better control.
For those who do get help from the diet, this new found symptom control may make you feel too fearful to move to the second stage of the diet and reintroduce foods. While you can certainly get all the nutrients you need from careful planning, not everyone that gets stuck in the elimination phase is going to eat enough variety of healthy nutritious foods.
Migraine, when poorly controlled, has a way of shrinking our lives. In a different and more subtle way, restricted diets can also diminish our lives by making us too fearful to participate in social situations, attend gatherings with friends and family and check out the local restaurants for fear of what may be on the menu.
For some people, the degree of planning, preparation and cooking is just too much for their current circumstances. The required changes may be impractical for them or too stressful. Fortunately, there are other aspects of the Treatment Pie that can also be very effective in reducing migraine attacks.
The worrisome
Elimination diets, including HYH, are intended to be temporary. They are not supposed to be long-term.
A small number of people stay on the restricted diet when it is clearly not working. Their attack frequency and intensity are unchanged after months of eating according to the plan yet they keep eating the same way while acknowledging that they really miss the foods they have been avoiding.
Some people combine the migraine elimination diet with other diet restrictions like gluten-free, dairy-free, keto or a vegan diet. The multiple restrictions can take its toll on the person’s overall health and wellbeing. Further, it’s not likely that all those restrictions will ultimately help the person control migraine.
Instead of spending time and energy seeking symptom control in other ways, they continue with diet as they feel like they failed somehow. Some may look for further food restrictions when their main attack triggers are not related to food. It can be very hard to try to convince someone to move on as they seem very attached to dieting their way to migraine relief.
The migraine diet has a bad reputation with some doctors as they see some patients that get stuck in the above ugliness and dismiss the advice to liberalize their diets.
Disordered eating?
I’m a registered dietitian focused on helping people with migraine and not a specialist in eating disorders, but I’m troubled at times by what I read on social media channels. Some people seem to be obsessed with their diet. When someone is embarking on a new way of eating, it is understandable and typical to be consumed with thoughts and questions about their next few meals, but this way of thinking should be short-term. There should be a sense of ease that occurs rather than anxiety over what to buy from the store or self-blame over what was eaten that might have caused the current migraine episode.
Orthorexia is defined as an obsession with healthy eating. People with orthorexia become so fixated with their definition of what is healthy for them that they end up damaging their own well-being. While people with migraine may be dieting as an intervention to help manage migraine attacks, there comes a point at which some cross the line into what is likely disordered eating.
Please read the warning signs of orthorexia and seek professional help if you think the criteria may apply to you.
What to do if you are feeling better but too afraid to add foods back
If you aren’t already in our Facebook group, consider joining and taking advantage of the supportive and upbeat community. Make a post about your dilemma and ask for some hand-holding or a buddy that is in the same situation.
Usually, the suggestion is to choose a food that you really miss to challenge first. It’s ok to take baby steps toward a more varied, balanced diet with more wholesome foods. If you haven’t read our blog with excellent tips on reintroducing foods, now’s the time.
If you think you might have disordered eating, please contact your doctor.
What to do if you have unsuccessfully tried to add foods back?
This is mixed news. This means you are significantly better while following the HYH or Charleston diets. Clearly, that is something to celebrate. However, some people may find that many of the foods they have tried to add back have resulted in migraine attacks.
If you find yourself in this situation please don’t despair as there is a good chance you will be less sensitive as your migraine condition improves over time. To make sure you are getting enough essential nutrients, focus on eating lots of colorful, nutrient dense foods. Technically, the diet can be safe long-term assuming that your circumstances and taste buds allow you to prepare and eat a good variety of foods. BUT, this assumes a lot.
We discourage staying on the HYH diet strictly. Many evolve to a sort of personalized “HYH/Charleston light” way of eating which allows more variety and better choices especially when eating away from home. Find your own personalized version of HYH and continue to try to add foods back.
Additionally, taking a good multivitamin/mineral supplement should help you on days when you aren’t getting enough nutrients in your diet.
You may also benefit from taking supplemental magnesium and Vitamin D3 as it’s often hard to get enough in our diet under the best of circumstances. As a person living with migraine, you may need a little more of these nutrients than the average person.
Personally, the migraine diet helped me immensely. During perimenopause my attacks became uncontrollable. I discovered foods that I used to eat all the time triggered attacks. My diet evolved to “HYH-light” where I was enjoying pizza, a little deli turkey and all plain breads and some condiments. It’s amazing how much freedom that gave me in addition to it being mentally and physically healthier. Fortunately, menopause allowed me to eventually add all my previously-triggering foods back into my life. Aged cheeses, yogurt and onions and I and all good friends again in small to moderate amounts.
What to do if you aren’t better on the diet?
So, you’ve been doing the diet for months. You haven’t been perfect (or maybe you have) but you aren’t better. First, kudos to you for the HUGE accomplishment. A migraine elimination diet can be challenging. You may not have food triggers. And you might be bummed as you put so much time and effort in, but I urge you to look on the bright side. You have no reason to be down. The purpose of a migraine elimination diet is to determine IF you have food triggers and, if so, pinpoint what they are. But, you may determine you don’t have any food triggers…and that knowledge IS success, not failure! You can resume eating those wholesome, delicious foods and fully participate in social gatherings again!
When an intervention does not work as anticipated, we always need a plan for what is next. I firmly believe that food can help many people with migraine and other chronic conditions. Certain diets may help reduce inflammation, specifically neuroinflammation.
HYH/Charleston are most useful in discovering food triggers not general inflammation. There are a number of evidence-based diet approaches that may help you reduce migraine attack frequency, intensity and duration. Below, I discuss 3 ways of eating PLUS my recommended BEST diet for migraine prevention that I believe most of us should be moving toward.
A few words about prodrome versus true trigger
It’s very common to hear people say they have strong cravings for sweets and salty snacks before a migraine attack. Chocolate is specifically mentioned quite often. Because of the timing of the craving, followed by the full migraine attack, many people point to the indulgence as the trigger. While this may be true for some, there is a very good chance that the the cravings-indulgence-attack sequence is really prodrome of migraine followed by the headache/nausea/etc. phase that is most recognizable. This article explains the phases of migraine well and you can see “food cravings” clearly mentioned.
During the reintroduction phase of the elimination diet, it will hopefully become more clear. Fingers crossed for you that that chocolate is not a trigger.
Choose a diet that minimizes your inflammation
The following ways of eating can be helpful in managing migraine.
Keto
Keto is a known, evidence-based intervention to minimize migraine attacks. When you follow a ketogenic diet, your body switches from being a carb-burning machine to a fat-burning machine. To get yourself into ketosis, you have to follow a very low carbohydrate diet so your body has to switch to burning the fat you eat or the fat on your body as its steady fuel source.
Keto for migraine is one of my favorite approaches to managing migraine. I have written 2 blogs about it as it can be very helpful. Some people notice that by just limiting sugar and high-carb foods they find reduced migraine attacks. Full ketosis may or may not be necessary.
Fish
Eureka! An excellent study of diet that suggests what we should include in our diet rather than exclude! The very recent research showed a significant reduction in attack frequency and duration when eating a diet high in omega-3 fatty acids from fish (not omega-3 supplements). Of the 3 study groups, the one that had the best results also ate a diet that was low in omega-6 fatty acids from highly processed vegetable and seed oils.
You must read my article about the very positive relationship between fish oil and migraine.
Mediterranean
More and more, I hear of neurologists suggesting the Mediterranean diet rather than advice that frustrates me, “just eat healthy.” The term “eat healthy” means drastically different things to different people.
I think this advice is catching on as there are many good resources available for the eating Mediterranean style. Additionally, many neurologists with keen interest in migraine may also be aware of the study about eating fish.
If you do an internet search of the Mediterranean diet, you will get many different interpretations. This article about the diet is easy to read and very helpful. In general, the Mediterranean way of eating has these characteristics:
- use of olive oil instead of “vegetable oils”
- focus on eating fish high in omega-3 fatty acids
- eat lots of veggies
- enjoy whole grains close to their natural form (not pulverized into flours)
- snack on nuts
- enjoy fruit for desert
Of course, the above are the general guidelines. You can still follow the Mediterranean diet and include other meats, breads and confections occasionally. The point is to focus on the above 6 bullet points.
Bottom Line It! – What’s the best diet for migraine?
The best diet for migraine, and the one I believe we should all aspire to, has these 5 qualities:
- Mainly made up of minimally processed foods that look similar to how they appear in nature. The rationale is that these foods tend to be more nutrient-dense and have minimal amounts of potentially inflammatory ingredients like sugars and highly processed vegetable and seed oils.
- Limited in added sugars as sugar may cause fluctuations in blood sugar (a possible migraine trigger) as well as contribute to inflammation.
- Inclusive of a variety of foods from all colors of the rainbow, especially the deeper and brighter colors. These foods provide a variety of vitamins, minerals and other nutrients associated with improved health outcomes.
- Inclusive of seafood high in omega-3 fatty acids if agreeable with your taste buds, as per the fish oil study discussed above.
- Minimized personal food triggers if you can confirm them.
What if you need help deciding or implementing a migraine-friendly way of eating?
Eileen Zollinger and I have been providing migraine coaching services for several years. We have many happy clients. You deserve to feel your best. Consider investing in your health and wellness. If you are interested, read more about the services we provide through the About Us tab at the top of this page.