What is the difference between sinus headache, sinus migraine and migraine headache? As it turns out, not much. Your sinus headache is very likely migraine. The location of the pain, as well as some common symptoms between sinus headache vs. migraine, seems to be the main reason for misdiagnosis by patients as well as primary care doctors.
Sinus headache or sinus migraine, although widely used by the public, “experts in the fields of otolaryngology, neurology, and allergy have agreed that it is an overused and often incorrect diagnosis in the majority of patients.” (1) In fact, as much as 90% of the time, migraine is masquerading as sinus headache. (2)
It’s hard to imagine that 90% of the people who have what they think is a sinus headache are actually experiencing migraine, right? Years ago, I spent six months being treated for a sinus infection that I didn’t have before I was correctly diagnosed with chronic migraine. Unfortunately, that led to 18 years of chronic, intractable migraine. When you look at the symptoms that migraine and sinusitis (sinus infection) have in common, it becomes more clear.
** While Migraine Strong writes about the latest in migraine treatments, this is not medical advice. We are patient educators and all information you read should be discussed with your doctor.
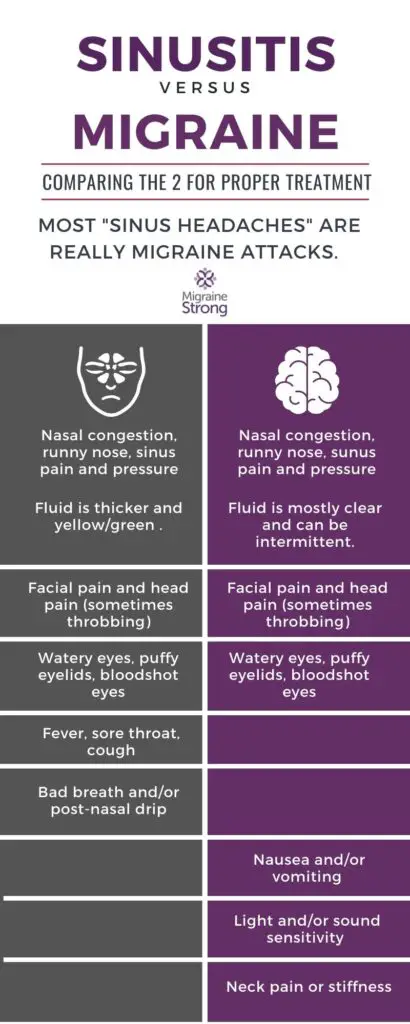
Symptoms sinus headache vs. migraine have in common
- Head pain
- Pain in eyes, nose, cheeks and forehead
- Watery eyes, puffy eyelids, bloodshot eyes
- Runny nose or congestion
- Tiredness
- Changes in weather bring on migraine attacks and frequently those with sinus headache will identify weather as a trigger for sinus symptoms
Looking at this list of symptoms I can say for certain that I have all of them with my migraine attacks. It makes perfect sense that having all of these symptoms and no clear cut diagnosis of migraine, most people would settle on sinus headache. Or if there was a history of migraine, maybe deciding they were having a sinus migraine attack.
However, “in clinical studies nearly 90% of participants with self-diagnosed or physician-diagnosed, sinus headache met criteria for IHS migraine-type headache and responded to triptan interventions in a manner similar to that witnessed in migraine. Consequently it is likely that most individuals seeking medical attention for sinus headache are, in fact, experiencing migraine.” (3)
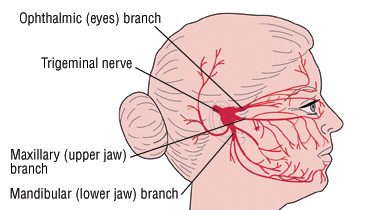
The trigeminal nerve and the role it plays in ‘sinus’ migraine
The Trigeminal nerve is also known as the fifth cranial nerve. It is involved in the activation of migraine. When you look at the image below, you can see why pain from a migraine attack can feel like an attack on the sinuses. Those sinus symptoms can be directly attributed to the irritation felt from the trigeminal nerve. We can see in the below image why migraine and sinusitis pain feel similar. The next step is figuring out how the two are different.
Signs of sinusitis or sinus infection not associated with migraine
- Bad smelling breath
- Nasal discharge – thick yellow or green discharge from the nose
- Post nasal drip – mucus running down the back of the throat
- Cough
- Sore throat
- Fever
- Potentially decreased smell
- Symptoms should resolve after 7 days for viral sinusitis or after a course of antibiotics for bacterial sinusitis.
These symptoms are not felt with migraine. These are signs of a viral or bacterial infection. Without these symptoms to accompany your sinus headache, chances are you fall into the 90% who are actually experiencing a migraine attack. (4)
A viral sinus infection will usually resolve within 5-7 days whereas a bacterial sinus infection will continue for 7-10 days and may actually get worse after 7 days. It’s important to see your doctor after a week if your symptoms don’t improve. (5) There are several risk factors that may make you more susceptible to developing sinusitis.
Risk factors for developing sinusitis
- Recent cold or respiratory infection
- Seasonal allergies
- Nasal polyps, small benign growths in the nasal passage that can lead to obstruction and inflammation
- Sensitivity to animal hair or dander, dust and pollen which leads to inflammation
- Deviated septum
If you have the risk factors listed above, you are at an increased risk for developing sinus infection or sinusitis. If you don’t have them, reconsider that maybe your sinus migraine or sinus headache is actually migraine.
Sinus headache vs. migraine – how to differentiate the two
Dr. Richard Lipton, from the Albert Einstein College of Medicine, developed the ID Migraine Questionnaire. This is a simple test to help determine if the headaches you are having are migraine. If you answer yes to two of these questions, your likelihood of having migraine is 93% and if you answer yes to all three the likelihood increases to 98%. This can help you to determine if the ‘sinus’ headache you are having is actually migraine.
- In the last three months, how disabling are your headaches; do they interfere with your ability to function? (Missing work, school and family activities?)
- Are your headaches ever associated with nausea?
- Are your headaches ever associated with sensitivity to light?
Migraine happens on a spectrum
The word disabling can be a stumbling block for some people when asked about their head pain. The symptoms involved with migraine, including pain, happen on a spectrum. Some people with migraine truly can’t function at all during an attack and must be in a very dark room with no noise to manage the symptoms…they are at the severe end of the spectrum. Others are affected by pain, light sensitivity and other migraine symptoms, still manage to function, but they are less productive and slower overall. That is still being impaired by headache or migraine, even if it doesn’t rise to the level of debilitating.
It’s an important point to discuss. I have talked to so many people who say they can’t have migraine because they don’t have to go to a dark room when they get their headaches. Or because ibuprofen helps with their symptoms, it can’t be migraine. Or even because their symptoms aren’t as bad as another person who has migraine, theirs can’t be migraine. All of those statements are untrue. Migraine happens on a spectrum with a mild and severe end. Understanding what type of headache you have will help you to treat it appropriately.
Some common symptoms of migraine
- Head pain (throbbing, could be one sided, made worse by activity)
- Sensitivity to light, sound and smell
- Dizziness, vertigo or a sense of being off balance
- Neck pain or stiffness
- Brain fog or inability to concentrate
- Nausea or vomiting
- Visual disturbances
- Numbness or tingling in the face or extremities
This list is not an exhaustive list of migraine symptoms. It is just to give you an overview of some of the symptoms that you could be feeling if you are experiencing a ‘sinus’ headache. Typically a migraine attack will last for approximately 4-72 hours. This is another indicator the head pain that was thought to be sinus related is actually migraine.
My personal experience with sinus headache vs. migraine
On a side note, I am experiencing a migraine attack today that was brought on by a weather system moving through my area and a significant drop in barometric pressure. Weather changes and migraine are often linked. I have incredible pressure and pain behind my eyes, cheeks, nose and forehead. I am light sensitive and the pain is sort of pulsating lightly. There is congestion in my nose and my eyes are slightly watering while my neck hurts and is very stiff. From long experience, I know this is a migraine attack and I have treated it as such, but with those symptoms, it’s very easy to see why people reach for ‘sinus’ medicine instead.
Why sinus medications may work to treat migraine attacks
One of the most common medications that people reach for when they have a ‘sinus’ migraine is a decongestant like pseudoephedrine, sometimes combined with an antihistamine like loratadine (Claritin-D). This decongestant medication acts as a vasoconstrictor which shrinks the dilated blood vessels within the nose, relieving congestion. The vasoconstriction can help with migraine pain as well. (7) The relief being felt from this sinus medication is, in part, what reinforces the idea of sinus headache.
If decongestants work reliably to relieve pain and are used infrequently, they can be enough to manage these ‘sinus’ migraine attacks. When they become several times weekly or a daily staple in treating sinus pain with/without congestion (migraine), there is a risk of developing rebound headache. To find out all about rebound, read our handy FAQ about it and this article about how to get out of rebound if you feel like you might be headed in that direction.
Why are so many undiagnosed?
Nearly half of those affected by migraine are never diagnosed. (6) Some patients will not see their doctor for what they deem to be ‘just a headache’, especially when it is responding to over the counter medications. However, the number of patients transitioning from episodic migraine (less than 15 days a month) to chronic migraine (more than 15 days a month, for 3 months) is 3% each year. (6) Understanding the type of headache (sinus headache vs. migraine) present is key to getting proper treatment and avoiding this transformation to chronic migraine.
Where to go from here
The goal of this article is to illustrate the differences and similarities between sinus headache, or more accurately, sinusitis (sinus infection) vs. migraine. To show that 90% of the time, the pain that is thought to come from a ‘sinus’ related headache is actually migraine and to encourage a new look at an old problem. This article is written from the patient advocate and educator perspective. This is not meant to be used as a diagnostic tool.
Make sure to contact a doctor well versed in headache medicine, a headache specialist, if you find that you are confused about the type of headache that you have. The American Migraine Foundation has a tool to help you locate a specialist in your area. Early diagnosis and appropriate treatment is key to getting control of migraine. Come join our private Facebook group if you would like to share your story or discuss more topics like this with others who understand.
Originally published December 3, 2020. Updated March 17, 2022.
References:
- https://pubmed.ncbi.nlm.nih.gov/23129234/
- https://americanmigrainefoundation.org/resource-library/sinus-headaches/
- https://pubmed.ncbi.nlm.nih.gov/15064062/
- https://ichd-3.org/wp-content/uploads/2018/01/The-International-Classification-of-Headache-Disorders-3rd-Edition-2018.pd 11.5.1 Headache attributed to acute rhinosinusitis Note 1
- https://health.clevelandclinic.org/killer-sinus-infection-how-to-tell-if-yours-is-viral-or-bacterial/
- https://medalerthelp.org/blog/migraine-statistics/
- https://americanmigrainefoundation.org/resource-library/acute-therapy-why-not-otc-options/
- https://www.health.harvard.edu/a_to_z/trigeminal-neuralgia-tic-douloureux-a-to-z
Great Article! I personal learned my sinusitis was food sensitivites to rose hips, some nuts and moldly environments.
Thanks for sharing! I had no idea there were so many common symptoms between the two.
Headaches, Migraines, Sinus issue and more are always a problem of the Trigeminal Nerve. There are 4 parasympathetic ganglia connected to the Trigeminal Nerve, the largest being the Sphenopalatine Ganglion or SPG. SPG blocks have over 100 year safety record for treating all of these issues. The SPG also contains sympathetic fibers arising from stellate ganglion and cervical sympathetic chain
It is often possible to treat or eliminate these problems with SPG Blocks. Self-Administered SPG Blocks (SASPGB) are very effective for treating these issues as well as anxiety. Originally described by Greenfield Sluder in 1908.
Great article. I have been diagnosed with Sluder’s Neuralgia on top of my 6 types of migraines. I had a car accident that caused my left frontal sinus to close. I have been sick for over a year with the facial pain of a sinus headache. I have a very slight deviation in the left side of my septum. It was excruciating when my gentle ENT probed the area and Benzocaine shots gave me 6 hours of relief.
I am going to have a procedure to shave down the septum.
I get a headache every month around the same time. I have been considering it a sinus issue, but this makes sense that it is actually a kind of migraine instead. It makes me feel sick to my stomach with nausea and diarrhea too, which isn’t typical for a sinus only issue.
Thank you for clearing all this up! It’s reassuring and very helpful. I truly appreciate Migraine Strong!
Thank you, I have been dealing with nasal congestion, sinus pressure, eye pain, facial pain throbbing, watery eye, sensitive to light, sound , neck pain, stiffness on my neck. This is a horrible feeling. I feel i can now relate to others. Sometimes, I feel drained mentally. Doctors , have not figured me out. But, we must me our own advocates and keep positive. I tried ( my client) told me . Boil water add ginger, 1/2 lemon, a tiny dash of honey. It helped me. I hate taking medicine. Yet, i am on a medication that makes me sleepy. To see if my migraines go away.
Lupita Uribe
Realtor / Fresno California
We love ginger and highly recommend it. If the lemon isn’t a personal trigger that sounds awesome!! I’ll link our blog on ginger for more information on it. -eileen The Gist About Ginger For Migraine Treatment