Constipation and I go way back. We have been lifelong companions though not friends. I can confidently say that after decades, I now have the upper-hand and rarely fall into the “strained” relationship. OK, pardon the pun. If you have been living with bouts of constipation as well as tension headaches or migraine, you probably want to know- can constipation cause headaches OR is it the reverse- does being prone to headache or migraine episodes cause constipation. As a registered dietitian diagnosed with migraine, I have spent quite a bit of time in this inquiry.
Anyone who has spent any time with people living with migraine is aware that gastrointestinal (GI) problems are common. Most frequently we hear about nausea and vomiting as it tends to be more disruptive. However, the effect of frequent or chronic constipation should not be poo-pooed (okay, I’ll stop). It turns out that yes, there is a connection between migraine and constipation. The lack of adult studies on the topic is frustrating but there is plenty of observational evidence in clinical practice.
Might this simply be correlation or might migraine be causing constipation? Or, perhaps constipation is actually causing headache and migraine.
** This article is written for information purposes only. It is not medical advice or a substitute for medical advice. Consult your doctor for any changes to your care plan.**
IBS, migraine and constipation
This type of GI upset is sometimes referenced as part of Irritable Bowel Syndrome – Constipation (IBS-C). According to a comprehensive article in the Annals of Gastroenterology, 10-20% of the adult Western countries have IBS symptoms. From that same article, it was estimated that IBS-C has an estimated prevalence of 35% of those with IBS.
Women are 3 times more likely to have constipation than men. And, as you probably already know, women have a much higher prevalence of migraine than men. But, maybe there is a causative link or behavior that leads to more frequent attacks of both. Might constipation cause migraine headache attacks? Maybe it’s part of prodrome (the first phase of migraine, before the full attack).
** This article is written for information purposes only. It is not medical advice or a substitute for medical advice. Consult your doctor for any changes to your care plan.**
What constipation is and what it is not
Constipation is defined as difficult or strained passing of stool or hard stool.
For some people it is normal for them to move their bowels twice per day, while others may skip a day or 2. In general, a doctor would consider you constipated if you had less than 3 bowel movements per week. Additionally, stool that is very hard or lumpy or stool that is broken into pellets or balls is a sign of constipation. If passing stool is causing a lot of strain, is painful or feels incomplete, that is considered constipation.
Can constipation cause headaches and migraine?
After quite a bit of time diving into this query about a constipation causing headache or migraine episodes, my opinion is that the two conditions are NOT merely associated. There is some evidence for constipation causing headaches. A good but small study about constipation and headache showed that the patients that were treated for constipation had fewer headaches. While some in the study had migraine, most participants had tension-type headache. But, some of the people with migraine were helped by intervening with osmotic laxatives (discussed below).
There are a number of theories but the constipation, headache and migraine link is likely a combination of the following factors:
1- The bi-directional gut-brain axis
The research about the gut-brain connection being part of a variety of medical conditions is very exciting. It seems obvious that there is a connection between our brain and GI tract as we are living proof. For instance, how strange is it that anti-nausea medications like Zofran and Compazine are also migraine medications when nausea isn’t even present. Or, for some people, a painful migraine attack comes to an end with vomiting or having a bowel movement.
Serotonin, migraine and constipation
Serotonin is a critically important neurotransmitter for our mental, emotional and physical health. It is considered one of the “happy hormones” and is primarily made in the GI tract.
For many people with migraine, abnormal activity of serotonin is thought to play a significant role in the cascade of biochemical changes that result in an attack. Some important medications we take for migraine impact our serotonin levels.
It turns out that serotonin also has important roles in the GI tract. Serotonin effects motility of the bowel, secretions into the bowel and the way we perceive sensations in the bowel. Perhaps the link between migraine and constipation has to do with altered metabolism of this important neurotransmitter.
As we age and go through hormonal changes like perimenopause and menopause, constipation can become more of an issue. Sometimes this coincides with depression, a common co-morbidity. Serotonin is the likely part of problem.
2- Medications and Supplements
Many of us are on medications for migraine or other medical conditions. Some of the more commonly prescribed medications with constipation as a side effect are anti-depressants (both SSRIs and tricyclic antidepressants), blood pressure medications like propranolol, and anti-nausea medications like Zofran.
Some people are prescribed opioids occasionally and those can certainly get us stopped-up quickly. Over-the-counter medications that are associated with constipation are antihistamines and antacids like Tums.
There have been many more queries about constipation since the release of the newer anti-CGRP migraine medications . A known side effect for some people is constipation that can be more than a passing nuisance. There are lots of neurologists that have had to bone-up on their knowledge of effective constipation remedies for our crowd.
Both iron and calcium supplements are known to be problematic. If you have been prescribed these by a doctor, continue to take them but work on the below tips to get things moving regularly again.
3- Stress
The connection between migraine and stress is well-known. Stress is often cited as the most significant trigger of migraine attacks. Did you know that stress is also associated with constipation? Stress can alter the hormones that specifically affect motility in the gut and slow things down.
4- Hydration, migraine and constipation
There is evidence that suggests that we need more hydration than the average person who does not have migraine. This alone may explain part of the migraine and constipation link. Checkout my blog about hydration and migraine.
Some people become constipated because they may drink very little each day. For other people, their colon may be over-achievers. One of the main jobs of our colon is to remove excess water. Perhaps your colon has a tendency to take away too much fluid and leave behind stool that is dry, lumpy and hard to move along.
5- Diet
Most people in the United States do not get enough fiber. For many who deal with debilitating migraine attacks and vestibular migraine, getting enough fiber may be especially challenging. Reaching for lower-fiber, prepared foods and highly processed foods is understandable when we aren’t feeling well. This isn’t a judgement or an excuse. It’s a reality of chronic illness.
6- Inadequate activity and exercise
When we are inactive, the natural and necessary muscle contractions that move food and stool through the GI tract slow down. If you are prone to frequent migraine attacks, your desire and ability to be active or exercise is likely impacted.
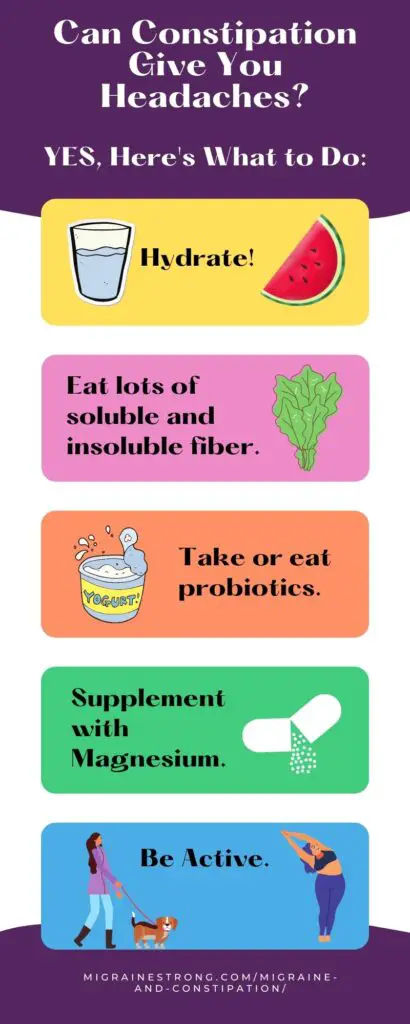
5 critical steps for constipation relief
1- Boost your water intake.
I know, I know, some of you may bristle at this advice. If you haven’t already read my article about the importance of hydration, please do so. This is a necessity to minimize both constipation and migraine.
Some of you may bristle for a different reason – you already drink plenty of water. Kudos to you for that!
2- Dietary Fiber
Boosting your fiber intake may not be news for you. As you might know, some forms of fiber can cause bloating and discomfort while others help speed things up, soften the stool and bring about relief. Let’s look at the different types and how they work.
Soluble fiber
Soluble fiber helps our digestion by serving as a bulking and softening agent. It is soluble in water and holds onto water from within the stool so it can move through the intestines. Examples of soluble fiber that are often helpful are found in oats and many fresh, whole vegetables and fruits.
Insoluble Fiber
Insoluble fiber is made softer inside the GI tract, but it does not dissolve in water. A helpful role it has is to add even more bulk to the stool so that the muscles along your GI tract can propel it toward its ultimate goal, your colon and ultimately, your commode. Somes foods high in insoluble fiber are nuts, beans, kale and quinoa.
3- Probiotics
Our GI tract is naturally loaded with a large variety of bacteria that is mostly helpful to our health. Having a good balance of the beneficial bacteria helps to keep the harmful bacteria in check. When we eat good sources of probiotics like fermented foods, it helps keep a healthy balance of beneficial bacteria. In addition to helping the healthy bacteria thrive with probiotics, eating foods high in both soluble and insoluble fiber help provide it our gut flora with valuable nutrients.
4- Activity! Inactivity is the enemy of both migraine and constipation.
As stated above, when you are active the muscles responsible for moving the contents of your GI tract forward contract more. If you want your GI motility to increase, boost your own movement.
For many of us with chronic conditions, exercise is hard. And, for some people, exercise may induce headaches or migraine attacks. This website is a great resource for getting you moving in spite of migraine.
5- Magnesium for constipation and migraine
Magnesium for migraine, especially magnesium glycinate, is a known help. It’s a very absorbable and the least likely form of magnesium to cause tummy trouble. But, magnesium citrate may be the workhorse that is best for you. Since constipation can cause headaches and migraine, why not take something that can do double-duty for you – help lessen your migraine attacks and help loosen your stools and make it easier to go.
We like Pure Encapsulations magnesium citrate and Natural Vitality Calm. It comes in flavored or unflavored options. You can also look for magnesium citrate in our supplement dispensary to receive a significant discount and free shipping with every $50 purchase.
When you need more help for migraine constipation
If increased hydration, boosting fiber and probiotics along with regular exercise aren’t getting you the results you are looking for, it’s probably time to try some over-the-counter intervention.
First, start slowly. Bombarding your colon with multiple types of laxatives may make you extremely uncomfortable and have unintended and embarrassing consequences.
I recommend trying products in this order. IMPORTANT– All of these products need you to drink additional fluids for them to work properly. Read and abide by the package instructions including calling your doctor if your symptoms continue.
Bulking agents
These products add fiber to your diet in a convenient beverage. Common brands include Fibercon, Metamucil, Citrucel, Benefiber. You may have to try a few to find the best one for you in terms of results and tolerance of potential gas and bloating. Read the ingredients and avoid the supplements that contain sugar-substitutes as they are migraine-triggering for some people.
Osmotic laxatives
Miralax (and generic versions) is a popular brand using polyethylene glycol to draw water into the GI tract to add bulk and soften the stool to make it easier to move through your body. Miralax is effective and tends to be well-tolerated and gentle. It may take a few days for this to start working. Because of the lack of taste, this product is popular and recommended by doctors often.
Saline osmotic laxatives
Like Miralax, this type of osmotic laxative works by pulling water into the GI tract but it does so using the mineral salts in different forms like magnesium citrate and magnesium hydroxide. Phillips’ Milk of Magnesia is a popular brand of magnesium hydroxide. Results are often faster with saline osmotic laxatives but they are less accepted due to the off putting taste.
Stool softeners
This type of medication works by causing the gastrointestinal tract to absorb water and soften the stool. Common brands are Colace and Correctol. Stool softeners usually take a few days to work and have been less prescribed by doctors over the years in favor of the osmotic laxatives.
Stimulant laxatives
The way that stimulant laxatives work is by stimulating contractions of the nerves and muscles along the GI tract. These drugs are widely available over-the-counter but they are recommended less often by doctors and pharmacists. There is a risk of becoming dependent on them if overused. Additionally, some people have significant cramping after taking them. This can make migraine and constipation that much more unpleasant. An advantage is that typically, the results are faster than with osmotic laxatives and stool softeners. Popular brands are Senokot, Ex-Lax and Dulcolax.
Knowing when you need “help from below” for constipation
Things are about to get a little more sensitive. I apologize in advance for the TMI (too much information), but it’s usually left out of articles on constipation. My goal is to give you practical advice as we are working under the assumption that constipation can cause headaches and migraine. You need relief from both!
When stool slows down in your GI tract or when you suppress the urge to move your bowels, your colon draws more water out of the stool. The colon is about 5 feet long so there is a lot of room for storage.
Your goal should be to easily pass poop that is similar in shape and firmness to a banana. Lumpy poops, hard pellets or poop balls are signs that the stool has been in your colon for a long time and too much water has been removed. For many people, if nothing is done the poop becomes a larger rounded mass like a tennis ball and can seem impossible to pass without tearing the anus. Let me help you avoid this!
Take a peek!
First, always glance in the toilet and see what you’ve produced. Was it an easy-to-pass smooth banana? Gold star! If it was lumpy, you probably still have time to help yourself by drinking more water, eating higher fiber foods and exercising. If you are uncomfortable and/or the stool was hard to pass, I suggest that you not wait longer and add a bulking agent.
When the stool is very difficult to pass, I suggest you enlist some “help from below” so that you don’t strain more and develop or worsen hemorrhoids or cause a tear and some bleeding. The hardened ball of dry poop can be helped out by making it slippery with a solid glycerin suppository or liquid glycerin suppository delivered by a convenient small bulb. This is a popular brand of liquid suppository designed for kids that should do the trick for adults when the solid suppositories are not helpful.
If you have noticed that your stool is chronically hard and difficult to pass, it may take a few weeks to notice a difference. You may have quite a lot of old stool that needs to come out of your colon. Remember, your colon is about ~5 feet long. Between your new focus on hydration, increased activity level, changes in diet and experimenting with different laxatives, you can find relief from migraine constipation as well as prevent it.
When to see a doctor
The above is designed as general helpful information. It is not medical advice nor meant to replace individualized attention from a doctor. There are times when individualized intervention is needed from a qualified medical professional.
This blog has been updated and refreshed with new content. It was originally published in September of 2020.
I have been practicing eating healthy and exercise to were it actually caused health problems. Btw to much of anything is bad. I was going to become a PT assistant but because of my age and concern for my back problems and headaches I choose nursing. Keto diet is a high fat low fiber diet? Good for cancer not for constipation? I have suffered from migraines since my first time at college in the 80’s and have notice constipation and relief go with the migraines. I am interested in more information on the topic. Also anyway I can help.
Sincerely
Michelle Reeves
Hi Michelle. Keto can be a good tool against migraine. I wrote about that topic recently, too. Constipation is a common complaint with keto but usually it happens more in the early stages. From experience, increasing hydration and making sure you are getting enough electrolytes is important to keep bowels moving along. And of course, magnesium has been shown to help migraine and can be a good supplement to take if constipation isn’t resolving quickly.
Hot coffee helps me fight constipation and migraine. I wish I had known this from birth. Resisting coffee, disliking the taste, a doctor ordered it with migraine prescription… Coffee helps, when all their drugs failed.
Learning to like it with creamer, I ran out and learned that helped more against both issues.
I have always had an issue with constipation . But now it seems every medication I take to help with my migraines …the side effect is always constipation.